Oct. 14, 2022
Developmental dysplasia of the hip (DDH) encompasses a spectrum of disorders related to abnormalities of the developing hip and includes frankly dislocated hips, instability and a shallow acetabulum. The current term defined by the American Academy of Orthopaedic Surgeons (AAOS) and the Pediatric Orthopaedic Society of North America (POSNA) emphasizes that DDH is not limited to congenital disorders but is an evolving condition that can change with growth and development.
"Asking families about their history of DDH along with the presence of breech position during pregnancy can identify which patients can benefit from a careful examination and hip ultrasound," says Todd A. Milbrandt, M.D., an orthopedic surgeon and the chair of Pediatric Orthopedics at Mayo Clinic in Rochester, Minnesota. "This approach can prevent the 'missed' hip dislocation."
DDH is a separate condition from neuromuscular hip dysplasia, which occurs most frequently in patients with spasticity. The cause of DDH is likely a combination of genetic and environmental factors. A strong association between the female gender and DDH has been shown, with 80% of those affected being female, according to a study in the Journal of the American Academy of Orthopaedic Surgeons. In addition, other risk factors include first born, breech position, a family history of DDH and oligohydramnios as supported by a study in The Journal of Bone & Joint Surgery.
Making the diagnosis in the newborn depends primarily on the hip exam, which generally should be performed routinely at each visit in infants. The baby should be examined while relaxed. The child should be undressed, and the diaper removed. The leg should be gently abducted and adducted. The sensation of the femoral head moving in, Ortolani sign, or out, Barlow sign, of the femoral head with a soft shifting or clunk should be the trigger for treatment or further imaging.
Infants with an unstable hip generally should be seen by a pediatric orthopedic specialist within 1 to 2 weeks for prompt treatment. Limited hip abduction on one or both sides is another physical exam finding that prompts ultrasound. In addition, ultrasound imaging also should be obtained at 4 to 6 weeks of age when any risk factors are in place, including a first-degree relative with hip dysplasia or history of breech intrauterine positioning. A low threshold for ultrasound is prudent to ensure early diagnosis and treatment. And it is helpful for providers to know that this is an ultrasound study that requires significant skill, as cited in a study published in the Journal of the American Academy of Orthopaedic Surgeons. Patients at 6 to 8 weeks of age with ultrasound abnormalities also generally should be referred for pediatric orthopedic evaluation.
"Hip ultrasounds are great screening tools for patients who have the risk factors noted above," says Dr. Milbrandt. "Patients with unstable hip examinations should be immediately referred without an ultrasound. However, patients with stable hip examinations and risk factors should obtain a hip ultrasound at 6 weeks of age."
As the child ages, the hip instability signs are no longer present. Changes in gait such as a limp or shortened limb is most common. Pain is not seen in toddlers with DDH. After 6 months of age, an anteroposterior pelvis X-ray is the best study to evaluate for hip dysplasia, and it provides more-reliable images than ultrasound. As the child ages, undiagnosed DDH will begin to cause pain as the forces across the joint become more abnormal.
For clinically unstable or dislocated hips, the optimal initiation of treatment with the Pavlik harness is as early as possible. It is successful in over 85% of the patients, according to results published in Orthopaedics & Traumatology: Surgery and Research. For the patient with mild ultrasound abnormalities, a stable hip and a normal clinical examination, treatment timing is controversial, as evidenced in a longitudinal study published in The Journal of Bone & Joint Surgery.
Left hip dislocation
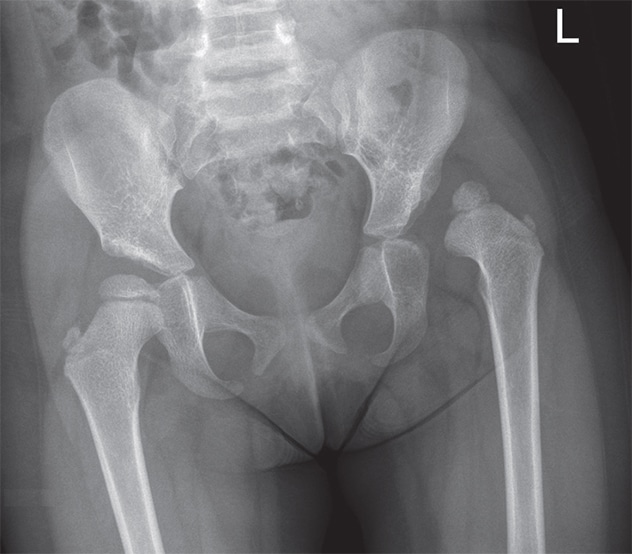
Left hip dislocation
Three-year-old female presenting with new diagnosis of left hip dislocation. The acetabular index on the left is increased and ossification of the femoral head is delayed.
Post-surgery
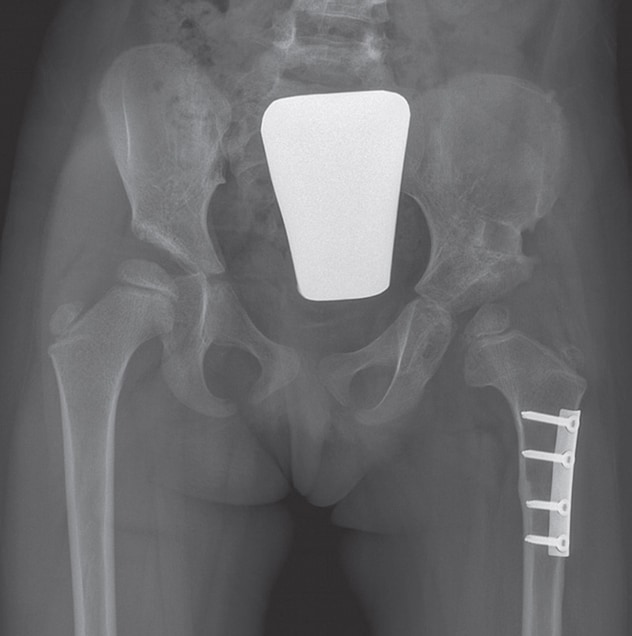
Post-surgery
Three-year-old female three months following open reduction, capsulorrhaphy and Pemberton osteotomy.
If bracing fails, then a closed reduction and spica cast application is performed around 6 months of age. As shown in a study published in the Journal of Pediatric Orthopaedics, some dislocated hips require a more invasive surgery to open the hip joint and reduce the hip. This can be coupled with either a cut in the femur or acetabulum. Some complex hips require making a 3D model, using techniques readily available at Mayo Clinic, to fully understand the anatomy to ensure a successful surgery, according to a study published in 3D Printing in Medicine.
"Using 3D printing for surgical planning and patient education is particularly helpful in pediatric orthopedic applications as these models are life-size and patient-specific," says Jonathan M. Morris, M.D., a neuroradiologist and the medical director of the 3D Anatomic Modeling Lab at Mayo Clinic. "This allows the surgeon to use the model to pre-procedurally plan in a controlled environment or, in many cases, rehearse the steps of the procedure on the 3D-printed model.
"As a leader in this space, Mayo Clinic's 3D printing for surgical planning and patient education is one of the many approaches available to our surgeons that allows them to take on cases with greater complexity," says Dr. Morris. "Additionally, it highlights the multidisciplinary collaboration between radiology and pediatric orthopedics — leading to better outcomes."
Hip dysplasia

Hip dysplasia
20-year-old with residual hip dysplasia and pain
Acetabular dysplasia

Acetabular dysplasia
Acetabular dysplasia in 20-year-old corrected with a periacetabular osteotomy
Older children also should be treated if they develop symptoms. As cited in a review in The Bone & Joint Journal, children older than 10 can be treated with periacetabular osteotomy, which is technically demanding but leads to powerful deformity correction. Sometimes periacetabular osteotomy is coupled with hip arthroscopy to ensure that any issues inside the joint also are addressed. This combination of procedures has been shown to decrease the rate of degenerative changes and delay hip replacement, according to a study published in The Journal of Bone & Joint Surgery. This surgery should only be performed by highly trained and experienced surgeons because complications can occur. Finally, if the hip can't be reconstructed because of DDH, a hip replacement in late adulthood, when it's performed by a high-volume academic center, can return function to a painful hip, according to results of a retrospective review published in Clinical Orthopaedics and Related Research.
DDH is a common condition with reliable nonoperative treatment options if detected early. Surgery is required for older patients with dislocated or unstable hips. The role of surgery for acetabular dysplasia in childhood is evolving and primarily driven by symptoms. The treatment options for DDH are expanding, and physicians are learning how to better assess the patient's anatomy, thus leading to the right intervention at the right time.
For more information
Vitale MG, et al. Developmental dysplasia of the hip from six months to four years of age. Journal of the American Academy of Orthopaedic Surgeons. 2001;9:401.
Garvey M, et al. Radiographic screening at four months of infants at risk for congenital hip dislocation. The Journal of Bone & Joint Surgery (British Volume). 1992;74:704.
Mulpuri K, et al. Detection and nonoperative management of pediatric developmental dysplasia of the hip in infants up to six months of age. Journal of the American Academy of Orthopaedic Surgeons. 2015;23:202.
Bin K, et al. Developmental dysplasia of the hip in neonates: Evolution of acetabular dysplasia after hip stabilization by brief Pavlik harness treatment. Orthopaedics & Traumatology: Surgery and Research. 2014;100:357.
Cashman JP, et al. The natural history of developmental dysplasia of the hip after early supervised treatment in the Pavlik harness. A prospective, longitudinal follow-up. The Journal of Bone & Joint Surgery (British Volume). 2002;84:418.
Holman J, et al. Long-term follow-up of open reduction surgery for developmental dislocation of the hip. Journal of Pediatric Orthopaedics 2012;32:121.
Leng S, et al. Anatomic modeling using 3D printing: Quality assurance and optimization. 3D Printing in Medicine. 2017;3:6.
Perry KI, et al. Hip dysplasia in the young adult: An osteotomy solution. The Bone & Joint Journal. 2013;95-B(suppl A):21.
Wyles CC, et al. Natural history of the dysplastic hip following modern periacetabular osteotomy. The Journal of Bone & Joint Surgery. 2019;101:932.
Amanatullah DF, et al. Similar clinical outcomes for THAs with and without prior periacetabular osteotomy. Clinical Orthopaedics and Related Research. 2015;473:685.
Refer a patient to Mayo Clinic.