March 05, 2015
The first description and subsequent adoption of transperitoneal laparoscopic adrenalectomy revolutionized the surgical management of small benign adrenal neoplasms. Laparoscopy resulted in reduced postoperative pain, less morbidity, shorter hospital stay and an earlier return to normal activity compared with open adrenalectomy.
Travis J. McKenzie, M.D., of the Department of Surgery at Mayo Clinic's campus in Rochester, Minnesota, says: "It is now readily accepted that laparoscopic adrenalectomy is the gold standard surgical approach, with open adrenalectomy being reserved for very large or malignant neoplasms. However, the traditional transperitoneal laparoscopic approach has notable limitations. The transperitoneal procedure involves approaching the adrenal glands from anterior, necessitating substantial organ mobilization to obtain access to the retroperitoneum. For example, laparoscopic left adrenalectomy requires mobilization of the left colon, spleen and pancreatic tail. This dissection can be complicated in the setting of intra-abdominal adhesions from previous operations."
CT scan from patient with a left adrenal mass
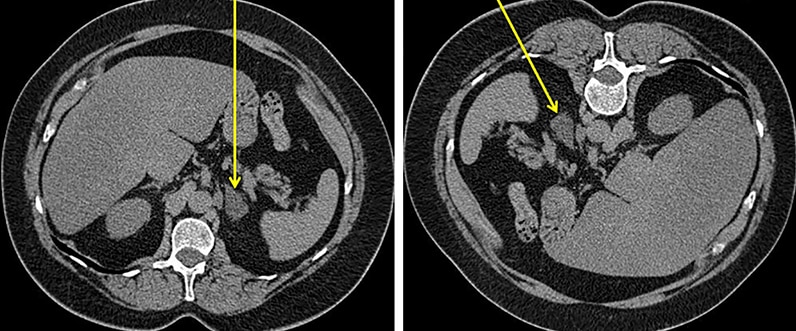
CT scan from patient with a left adrenal mass
The CT image on the left panel shows the angle of approach (yellow arrow) with transperitoneal laparoscopic adrenalectomy. The CT image on the right panel shows the retroperitoneoscopic approach (yellow arrow) to adrenalectomy.
Dr. McKenzie explains: "The retroperitoneoscopic adrenalectomy (RPA) approach involves placing the patient in the facedown (prone) position with the adrenal gland being approached posteriorly beneath the 12th rib. This approach allows direct access to the retroperitoneum and adrenal gland without the need for intra-abdominal organ mobilization.
"Furthermore, CO2 insufflation pressures in the retroperitoneum can be kept significantly higher than with traditional laparoscopy without limiting cardiac filling pressures. High insufflation pressures in the retroperitoneal space can limit troublesome bleeding that often occurs with the transperitoneal approach in which pressures are limited to 15 to 20 mm Hg."
There are currently no large prospective studies comparing laparoscopic transperitoneal and RPA approaches. Multiple retrospective series have demonstrated safety and efficacy of RPA. Martin K. Walz, M.D., of Kliniken Essen-Mitte in Germany, and colleagues published results of 560 retroperitoneoscopic adrenalectomies in 520 patients for neoplasms ranging from 0.5 to 10 cm in Surgery in 2006. Results were equivalent to contemporary series of transperitoneal laparoscopic adrenalectomies, including a minor morbidity of 14.4 percent and mortality of 0 percent with conversion to an open or laparoscopic approach in 1.7 percent of patients.
Dr. McKenzie highlights that: "All types of benign adrenal neoplasms may be accessible with the retroperitoneal approach, including both biochemically active and silent neoplasms. Relative contraindications to RPA include tumors larger than 7 cm and patients with BMI > 40 kg/m2. The working space is considerably smaller with the RPA approach, and therefore neoplasms larger than 7 cm are difficult to dissect safely. In addition, creation of the retroperitoneal working space can be limited by posterior compression secondary to a large pannus in an obese patient.
"RPA provides an excellent surgical option for select patients with benign adrenal neoplasms in the setting of previous abdominal operations where the traditional transperitoneal laparoscopic approach may be difficult. Furthermore, this approach may be utilized as a primary option with equivalent results to transperitoneal laparoscopy."
For more information
Walz MK, et al. Posterior retroperitoneoscopic adrenalectomy — Results of 560 procedures in 520 patients. Surgery. 2006;140:943.