Sept. 14, 2018
Hyperinsulinemic hypoglycemia is a disorder that can be very challenging to evaluate. Adrian Vella, M.D., an endocrinologist at Mayo Clinic in Rochester, Minnesota, says: "Once factitious disease has been excluded (that is, inappropriate use of hypoglycemic medication), insulinoma is the most likely cause of hypoglycemia. Noninvasive imaging studies such as abdominal ultrasound and computerized tomography with intravenous contrast can identify an insulinoma in approximately 75 percent of the cases.
"However, in the remaining instances, more invasive testing such as endoscopic ultrasound or selective arterial calcium stimulation test (SACST) is required. These tests alone or in combination have allowed virtually all insulinomas to be localized or regionalized preoperatively at Mayo Clinic since 1998."
The SACST has been of increasing interest to internists and endocrinologists since the relatively recent description of two distinct syndromes characterized by hypoglycemia, an abnormal SACST and abnormal islet morphology. Noninsulinoma pancreatogenous hypoglycemia syndrome (NIPHS) is a rare disorder characterized by postprandial hypoglycemia. A similar presentation has been encountered after Roux-en-Y gastric bypass (RYGB) and Nissen fundoplication.
Relationships among the three major arteries and regions of the pancreas supplied
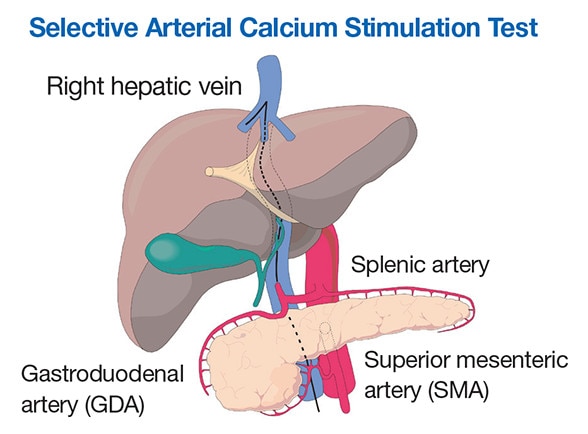
Relationships among the three major arteries and regions of the pancreas supplied
Graphic representation shows the relationships among the three major arteries (gastroduodenal, superior mesenteric and splenic) and regions of the pancreas supplied (head, uncinate process and tail, respectively).
James C. Andrews, M.D., a radiologist at Mayo Clinic in Rochester, Minnesota, says: "The SACST was developed by the late John L. Doppman, M.D., from the National Institutes of Health in response to the observation that intravenously administered calcium stimulates insulin release from insulinoma, but not from normal beta cells. The test requires cannulation of the femoral vein and artery with passage of a sampling catheter to the right hepatic vein for sampling for insulin and sequentially under fluoroscopic guidance, a catheter placed into the splenic, superior mesenteric and gastroduodenal arteries to allow injection of calcium gluconate into these arteries.
"Two 2015 publications by our group in Surgery and the Journal of Clinical Endocrinology and Metabolism have highlighted the importance of the arterial anatomy and regional perfusion when interpreting results of the SACST. The anatomy of the celiac axis and superior mesenteric artery is aberrant in approximately 40 percent of patients. Hence it is important to discuss the results obtained with the interventional radiologist performing the study. Such an approach significantly improves the sensitivity of localization for occult insulinoma."
Dr. Vella adds: "Previously a positive response to the injection of calcium was defined as at least a doubling or a tripling of the insulin level at more than one time point after the injection. However, consideration of the absolute value of peak insulin concentrations also is important in light of the pulsatile nature of insulin secretion where underlying endogenous insulin pulsatility may mimic a response to calcium injection.
Selective arterial calcium stimulation test results
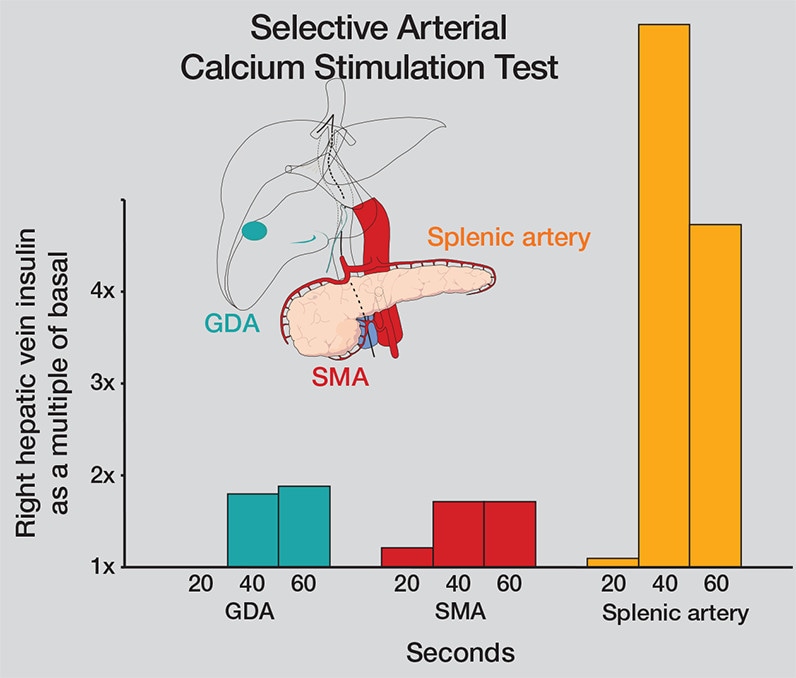
Selective arterial calcium stimulation test results
Results from selective arterial calcium stimulation test (SACST) show a less than twofold rise in right hepatic vein insulin levels when calcium is infused into the gastroduodenal artery (GDA) and superior mesenteric artery (SMA). The more than fourfold increase in right hepatic vein insulin concentrations when calcium is infused into the splenic artery (data shown in orange) is diagnostic of an insulinoma in the tail of the pancreas.
"A recent analysis of our experience with SACST suggests that positive territories usually exhibit a greater than fourfold response from baseline concentrations and the peak insulin concentrations observed with insulinoma are higher than those observed in subjects with NIPHS or post-RYGB hypoglycemia."
Dr. Vella concludes: "Continuing experience with SACST at our institution has reinforced the utility of the test in the management of hypoglycemic disorders when performed selectively. Close communication between the endocrinologist and the interventional radiologist also is important to interpret the results correctly and manage the patient appropriately."
For more information
Thompson SM, et al. Impact of variant pancreatic arterial anatomy and overlap in regional perfusion on the interpretation of selective arterial calcium stimulation with hepatic venous sampling for preoperative localization of occult insulinoma. Surgery. 2015;158:162.
Thompson SM, et al. Selective arterial calcium stimulation with hepatic venous sampling differentiates insulinoma from nesidioblastosis. Journal of Clinical Endocrinology and Metabolism. 2015;100:4189.