April 01, 2016
Individuals presenting to the emergency department with chest pain first undergo risk assessment and diagnostic testing to rule out life-threatening entities such as acute coronary syndrome (ACS), pulmonary embolism and aortic dissection. Among patients with suspected ACS, spontaneous coronary artery dissection (SCAD) is an increasingly important nonatherosclerotic cause of acute myocardial infarction (MI) and sudden cardiac death.
Increased awareness and improved imaging modalities suggest that SCAD, previously considered rare, is more common than appreciated. Novel use of online patient communities to catalyze research efforts and recruit patients with SCAD to the Mayo Clinic SCAD registry has substantially increased understanding of this condition, which is the most common cause of MI in pregnancy and the peripartum period and may account for up to 40 percent of MI in women younger than 40 years.
The development of atherosclerotic coronary artery disease (CAD) is understood to be due to the interplay of genetic and lifestyle factors that leads to endothelial plaques that may become unstable or occlusive, whereas the pathogenesis of SCAD is distinct from CAD.
"The demographic profile of individuals with SCAD markedly differs from those with atherosclerotic disease in that these patients are typically young women without conventional risk factors for CAD," according to Sharonne N. Hayes, M.D., a cardiologist at Mayo Clinic in Rochester, Minnesota.
More than 80 percent of patients with SCAD are female, with a mean age of 42 years at the index event, up to a quarter of which occur in the peripartum period. Associated factors include:
- Nonatherosclerotic systemic vasculopathies, especially fibromuscular dysplasia
- Extreme stress, emotion or exercise
- Connective tissue disorders
- Monogenetic mutations such as the vascular type of Ehlers-Danlos syndrome (formerly type IV) or Marfan syndrome (less commonly)
Patients with SCAD at Mayo Clinic undergo comprehensive vascular imaging; 66 percent of this population has evidence of extracoronary vascular abnormalities.
The presentation of SCAD mimics that of other acute coronary events; therefore, a high index of suspicion is required to make the diagnosis. Like other ACS, symptoms and signs of SCAD include electrocardiographic findings of non-ST or ST elevation myocardial infarction, elevated cardiac biomarkers, regional wall motion abnormalities, ventricular arrhythmias, and sudden cardiac death. Coronary angiography should be performed immediately if SCAD is suspected.
"SCAD may present angiographically with the appearance of a false lumen created by intimal dissection," says Rajiv Gulati, M.D., Ph.D., an interventional cardiologist at Mayo Clinic in Rochester, Minnesota. "However, more commonly, SCAD presents with intramural hematoma, which causes luminal compression."
Coronary angiogram and OCT of intramural hematoma
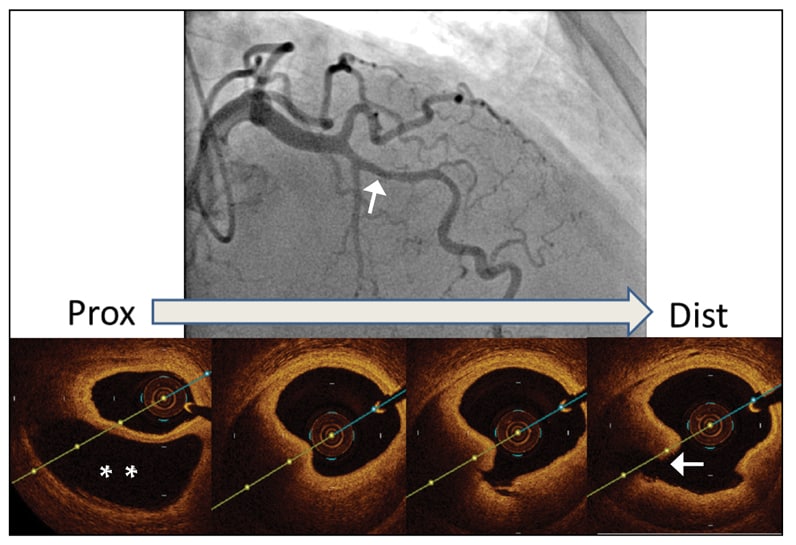
Coronary angiogram and OCT of intramural hematoma
Top. Coronary angiogram of a 49-year-old woman who presented with an acute coronary syndrome in the absence of atherosclerotic risk factors. The arrow indicates focal smooth stenosis in the mid left anterior descending artery. Bottom. Intravascular optical coherence tomography (OCT) reveals intramural hematoma causing compression of the coronary lumen as the reason for stenosis (asterisks, lower left panel), with an absence of intraluminal plaque. Sequential OCT frames moving distally indicate separation of the intima from the media (arrow, lower right panel).
This appearance may mimic vasospasm, mild atherosclerosis or "normal coronaries" and be difficult to visualize with angiography alone. Therefore, it is critical in these patients to consider intravascular ultrasound or optical coherence tomography to make the diagnosis. Correct diagnosis is essential, as management differs from recommended management of ACS due to atherosclerotic disease.
Other angiographic clues to SCAD include the absence of atherosclerosis or the presence of coronary artery tortuosity. "Coronary tortuosity is markedly more common in patients with SCAD compared with controls," says Dr. Gulati. Additionally, more severe tortuosity is associated with higher rates of recurrent SCAD.
Intriguingly, individuals with ACS due to SCAD who undergo percutaneous interventions (PCIs) have markedly higher rates of complications compared with those with CAD. In a retrospective series, 13 percent of patients with SCAD presenting with normal or near-normal blood flow required emergency coronary artery bypass graft surgery due to catastrophic complications from PCIs. This observation combined with the substantial rate of spontaneous vascular healing suggests a role for conservative management in stable patients with SCAD who have preserved coronary flow.
Empiric medical management (single antiplatelet agent, beta blocker, angiotensin-converting enzyme inhibitor therapy if appropriate) and close observation are recommended in these individuals. Because dissection may progress early in otherwise stable patients, four to five days of inpatient monitoring is recommended.
Recurrence rates of up to 20 percent at 10 years underscore the need for long-term management and follow-up. While specific SCAD recommendations cannot be made because long-term data are lacking, individuals benefit physically and emotionally from participation in cardiac rehabilitation programs.
Depression and anxiety are common after an event and should be recognized and treated. Nitrate-responsive chest pain also is common and often responds favorably to long-acting nitrates or calcium channel blockers.
As many patients with SCAD have a history of extreme physical activity immediately prior to their index event, it seems prudent to advise against high-level competitive athletics, extreme exertion or bodybuilding.
The high incidence of events associated with the peripartum period implicates a hormonal role, and women with SCAD are advised to avoid pregnancy and hormonal contraceptives. Empiric low-dose aspirin is recommended in these individuals.
Patients who have received a stent should receive dual antiplatelet therapy. Additional pharmacologic therapy should target non-SCAD conditions if present such as hypertension or hyperlipidemia. Routine statin therapy is not recommended, as it has been associated with an increased risk of recurrent SCAD.
Medical genetics evaluation is advised in these patients. "Although several monogenic mutations associated with vascular pathology have been identified in patients with SCAD, no mutations specific to SCAD (or fibromuscular dysplasia) have been identified to date," says Timothy M. Olson, M.D., a pediatric cardiologist at Mayo Clinic in Rochester, Minnesota. The Mayo Clinic SCAD registry has developed a Virtual Multicenter SCAD registry, which includes a DNA biorepository of blood samples from patients and first-degree relatives. Of the over 525 consented female SCAD participants, 98 percent have provided DNA samples.
Preliminary whole-exome sequencing data from a pilot study of 28 sporadic SCAD family trios and an affected sibling pair have revealed the following:
- SCAD is a genetically heterogeneous disorder.
- Mutations in genes for thoracic aortic aneurysm and dissection do not appear to be a common cause for SCAD.
- Four plausible candidate genes implicate perturbed Rho signaling, angiogenesis and actin cytoskeletal integrity as potential underlying factors in SCAD susceptibility.
This sequencing endeavor is a key component in the investigation of cardiac disease in young women.