Panorama general
Un hígado sano comparado con un hígado con cirrosis
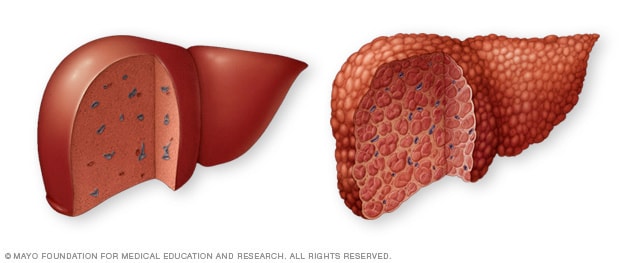
Un hígado sano comparado con un hígado con cirrosis
Un hígado sano (izquierda) no muestra signos de cicatrices. En un hígado con cirrosis (derecha), el tejido cicatricial reemplaza el tejido hepático sano.
El hígado
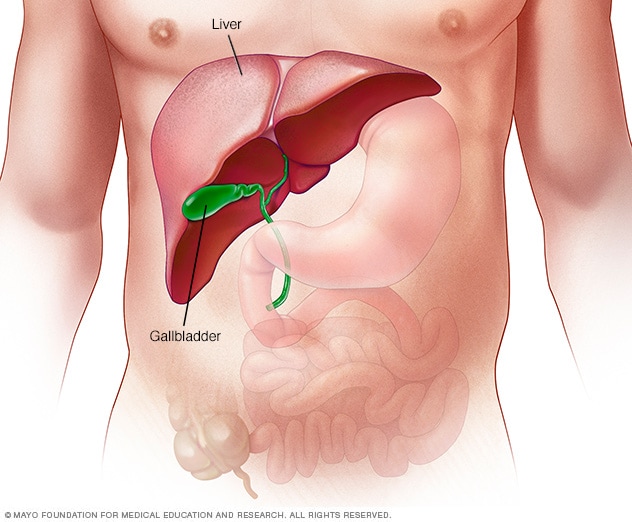
El hígado
El hígado es el órgano interno más grande del cuerpo. Tiene un tamaño similar al de una pelota de fútbol americano y se ubica principalmente en la parte superior derecha del abdomen, debajo del diafragma y encima del estómago.
The model for end-stage liver disease (MELD) score helps decide how urgently someone needs a liver transplant in the next three months. The score ranges from 6 to 40. A person with a higher score needs a liver transplant sooner than does a person with a lower score.
MELD scores are used for people age 12 and older who have liver disease. Healthcare professionals use the MELD score to predict a person's risk of dying while waiting for a liver transplant. This is known as mortality risk.
MELD scores help rank people on the transplant list so the people who are sickest are offered transplants first. MELD scores can go up or down while waiting for a transplant.
Liver transplant is a treatment option for some people with advanced liver disease. Liver decompensation or liver failure may happen quickly or slowly over months to years. Liver decompensation happens when the liver, scarred from a condition called cirrhosis, starts to lose its ability to function.
Cirrhosis is advanced scarring of the liver caused by a variety of liver diseases. As cirrhosis gets worse, more and more scar tissue forms, making it difficult for the liver to do its job. Major causes of cirrhosis that may lead to chronic liver failure and the need for liver transplant include:
- Viral hepatitis, including hepatitis B, C and D.
- Alcohol-associated liver disease, which causes damage to the liver from drinking excessive amounts of alcohol.
- Metabolic dysfunction-associated steatotic liver disease, a condition in which fat builds up in the liver, causing inflammation or liver cell damage. This condition was formerly known as nonalcoholic fatty liver disease.
- Genetic conditions that affect the liver.
- Diseases that affect the bile ducts, the tubes that carry bile away from the liver.
The liver damage caused by cirrhosis generally can't be undone. But if liver cirrhosis is diagnosed early and the cause of the scarring is treated, further damage can be limited.
People who have complications of cirrhosis, known as decompensated cirrhosis, likely need a liver transplant. Although liver transplant may treat sudden liver failure, it is more often used to treat decompensation from chronic liver disease.
Por qué se hace
The MELD score helps healthcare professionals predict how likely it is that someone with liver disease will die while waiting for a liver transplant. This is known as mortality risk. The higher the MELD score, the more urgently a person needs a new liver.
But the MELD score alone might not tell the whole story. Some people with certain complications may qualify for MELD exception points. These complications aren't taken into account in the MELD scoring system but they can be serious, lowering a person's chance of survival.
For example, a person who has liver cancer may qualify for MELD exception points regardless of MELD score. MELD exceptions improve a person's chance of getting a liver transplant sooner.
Riesgos
A MELD score is based on certain blood tests. Blood tests are typically safe. But there is some risk. You may:
- Bleed or bruise where the needle went into your vein.
- Feel discomfort.
- Feel lightheaded or dizzy.
Serious liver disease can cause anxiety, depression, sleep disorders and issues with everyday activities. A high MELD score may reflect both physical and mental well-being. Your healthcare team may schedule other tests or treatment to help support you.
Qué esperar
Healthcare professionals put the results of three blood tests into an online calculator to get a MELD score:
- International normalized ratio (INR). This test checks how well your blood clots. If the INR is too high, it means that your blood is clotting more slowly than it should. This may be a sign that liver disease is getting worse.
- Serum creatinine. The serum creatinine test helps check how well your kidneys work. Your liver makes creatine, a chemical important for muscle health. Creatine is converted to creatinine, which is a waste product made from the breakdown of protein and muscle tissue. Typically, the kidneys remove creatinine from the blood. As the liver gets sicker, it makes less creatine.
- Serum bilirubin. The bilirubin test checks the level of bilirubin in your blood. Your liver makes bilirubin when it breaks down red blood cells. Too much bilirubin causes jaundice — a yellowing of the skin and whites of the eyes — and may be a sign that liver disease is getting worse.
Healthcare professionals also may include other factors to determine a MELD score:
- Serum sodium. This blood test checks the level of sodium in your blood. Sodium helps balance the amount of water that's in and around your cells. Cirrhosis may cause your body to hold onto more water than it needs. Too much water and not enough sodium causes fluid buildup. Swelling in the belly is called ascites, and swelling in the legs, feet or ankles is called edema. Too much sodium can cause serious health concerns such as confusion or seizures.
- Serum albumin. This blood test checks the level of albumin in your blood. Your liver makes albumin, which is a protein that helps control fluid and swelling. Low albumin levels may be caused by liver disease.
- Sex assigned at birth. Creatinine is affected by how much muscle you have. Women typically have less muscle than do men, so their creatinine levels are often lower. Studies have shown that women were more likely than men to die while waiting for a transplant. The MELD score formula was changed to give women extra points to help improve the chances that they get the transplants they need.
For children younger than 12 years old, healthcare teams use the pediatric end-stage liver disease (PELD) score. The PELD score uses some of the same blood tests as the MELD score, such as INR, bilirubin and albumin. The PELD score also includes a child's height and weight. Some children also may qualify for exception points.
Resultados
The result of your MELD score helps your healthcare team tell how urgently you need a liver transplant.
Your health can change while you wait for a liver transplant. This can cause your MELD score to go up or down. That's why your healthcare team rechecks your MELD score.
The chart explains what the MELD score means, what to do and how often your MELD score is rechecked:
| MELD score |
What to do |
MELD score recheck |
6 to 10:
You have liver disease. |
Talk with your healthcare team about how to treat your liver disease. |
Check in 1 year. |
11 to 18:
Your liver disease is getting worse. |
Together, you and your healthcare team use an online calculator to determine your MELD score and talk about your liver transplant options. |
Check in 3 months. |
19 to 40:
You have serious liver disease. |
Together, you and your healthcare team use an online calculator to determine your MELD score and talk about your liver transplant options. |
19 to 24:
Check in 1 month.
25 to 40:
Check every 7 days.
|
| Based on Bambha K, et al. Model for end-stage liver disease (MELD). https://www.uptodate.com/contents/search. Accessed Aug. 7, 2025; BMC Musculoskeletal Disorders. 2023;24:310; Evidence-Based Practice of Palliative Medicine. 2023; Journal of Clinical Medicine. 2024;13:4275; The Lancet. 2021;398:1359; Organ Procurement and Transplantation Network. |
Typically, people with MELD scores of 15 or higher are more likely to live longer if they receive new livers. This is known as life expectancy.
One study calculated how many extra years a liver transplant could provide:
| MELD score |
Extra years gained with a liver transplant |
| 16 to 20 |
1.5 extra years |
| 21 to 25 |
3.5 extra years |
| 26 to 30 |
5.8 extra years |
| 31 to 34 |
6.9 extra years |
| 35 to 40 |
7.2 extra years |
| Source: American Journal of Transplantation. 2018;18:1231. |
Talk with your healthcare team about your liver condition and treatment options. They want to help you any way they can.
Oct. 28, 2025