Descripción general
Cáncer de hígado
Cáncer de hígado
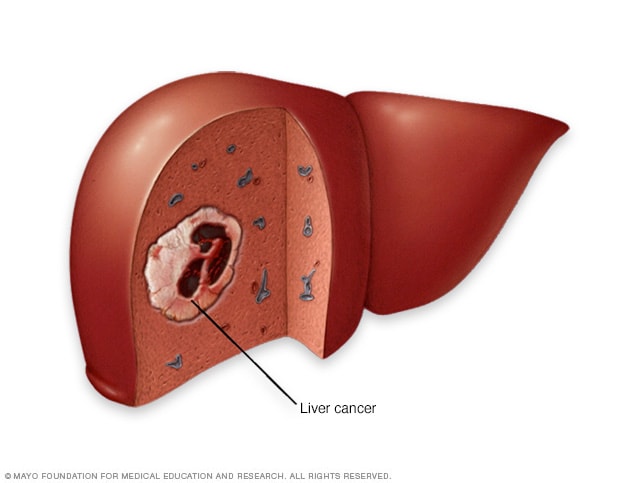
El cáncer de hígado comienza en las células del hígado. La forma más común de cáncer de hígado comienza en las células llamadas hepatocitos. Este tipo de cáncer se conoce como carcinoma hepatocelular.
El carcinoma hepatocelular es un tipo de cáncer que comienza como una proliferación de células en el hígado. El hígado es un órgano ubicado justo debajo de la caja torácica, del lado derecho del abdomen. Ayuda al cuerpo a digerir los alimentos y eliminar los desechos, entre otras funciones.
El carcinoma hepatocelular es el tipo más común de cáncer de hígado. Comienza en las células del hígado llamadas hepatocitos. El carcinoma hepatocelular se presenta con mayor frecuencia en personas con afecciones hepáticas crónicas, como cirrosis a causa de infección por hepatitis B o hepatitis C.
El carcinoma hepatocelular ocurre cuando una enfermedad hepática u otra causa altera las células del hígado. Estos cambios hacen que las células produzcan muchas más células afectadas por la enfermedad, que forman un tumor. El tumor puede dañar el tejido sano del hígado y crecer hacia los vasos sanguíneos cercanos. Las células pueden desprenderse y diseminarse a otras partes del cuerpo.
El carcinoma hepatocelular es uno de los tipos de cáncer más graves. Es posible que no cause síntomas de inmediato, lo que permite que crezca sin ser detectado. También suele aparecer en personas con enfermedad hepática grave, lo que puede dificultar el tratamiento.
El tratamiento depende en gran medida de la etapa del cáncer y del funcionamiento del hígado. El tratamiento del carcinoma hepatocelular puede incluir cirugía para extirpar el cáncer o un trasplante de hígado. Otros tratamientos pueden incluir ablación, embolización, radioterapia, inmunoterapia y terapia dirigida.
El carcinoma hepatocelular se diferencia de otro tipo de cáncer de hígado llamado colangiocarcinoma intrahepático. Este último comienza en los conductos biliares dentro del hígado, no en el tejido hepático. Ambos son tipos de cáncer de hígado, pero tienen factores de riesgo y tratamientos distintos. Otro tipo de cáncer de hígado llamado hepatoblastoma afecta principalmente a niños pequeños. Todos estos tipos forman parte de las neoplasias malignas del hígado, que es un término médico para cáncer en el hígado.
Tipos
El carcinoma hepatocelular no se clasifica en tipos. A veces, el carcinoma fibrolamelar se describe como un subtipo o variante del carcinoma hepatocelular, porque se cree que ambos comienzan en los hepatocitos. Sin embargo, el carcinoma fibrolamelar se comporta de manera diferente a la mayoría de los carcinomas hepatocelulares. Los profesionales de atención médica no están de acuerdo sobre si el carcinoma hepatocelular y el carcinoma fibrolamelar están relacionados o no.
El carcinoma fibrolamelar aparece con mayor frecuencia en adultos jóvenes que no tienen una enfermedad hepática. Por lo general, se trata con cirugía. A igual que la mayoría de los carcinomas hepatocelulares, el carcinoma fibrolamelar no suele causar niveles altos de alfafetoproteína en la sangre.
Productos y servicios
Síntomas
El carcinoma hepatocelular podría no causar síntomas que se noten de inmediato. Esta enfermedad ocurre con mayor frecuencia en personas con cirrosis, que es la formación de cicatrices en el hígado, a causa de una infección por hepatitis B o hepatitis C. En estas personas, los síntomas del cáncer podrían ser los mismos que los de la cirrosis.
El carcinoma hepatocelular no causa síntomas en las etapas iniciales. Un profesional de atención médica podría detectar signos tempranos de la enfermedad, como los siguientes:
- Resultados más altos de lo esperado en un análisis de sangre que busca alfafetoproteína, que puede realizarse como parte de un examen de detección del cáncer de hígado en personas con alto riesgo de la enfermedad.
- Nódulos, que son tumores en el hígado, que podrían detectarse mediante una ecografía realizada como parte del examen de detección del cáncer de hígado.
Si aparecen signos y síntomas del carcinoma hepatocelular, generalmente significa que la enfermedad está avanzada. Los síntomas pueden ser los siguientes:
- Pérdida de peso involuntaria.
- Pérdida del apetito.
- Dolor en la parte superior del abdomen.
- Un tumor en el abdomen.
- Color amarillento en la piel y en la parte blanca de los ojos. Esto se llama ictericia. Sucede cuando una sustancia llamada bilirrubina se acumula en la sangre.
¿Cuándo consultar a un médico?
Programa una cita con un médico u otro profesional de atención médica si tienes algún síntoma que te preocupa.
Causas
Las principales causas del carcinoma hepatocelular son la cirrosis, que es la formación de cicatrices en el hígado, y una infección por el virus de la hepatitis B o el virus de la hepatitis C. Sin embargo, no todas las personas con este tipo de cáncer tienen una afección hepática grave. No está claro cuál es la causa del carcinoma hepatocelular en quienes no tienen una enfermedad hepática.
El carcinoma hepatocelular ocurre cuando los hepatocitos, que son las células del hígado, presentan cambios en su ADN. El ADN de una célula contiene las instrucciones que le indican lo que debe hacer. En las células sanas, el ADN da las instrucciones para que crezcan y se multipliquen a un determinado ritmo. Las instrucciones les indican a las células que deben morir en un momento determinado. En el caso de las células cancerosas, los cambios en el ADN hacen que las instrucciones sean diferentes. Los cambios les indican a las células cancerosas que crezcan y se multipliquen rápidamente. Las células cancerosas pueden seguir viviendo más allá de lo que vivirían las células sanas. Esto causa un exceso de células.
Las células cancerosas forman una masa que se conoce como tumor. El tumor puede aumentar de tamaño hasta invadir y destruir el tejido corporal sano. Con el tiempo, las células cancerosas pueden desprenderse y diseminarse a otras partes del cuerpo. Cuando el cáncer se disemina, se llama cáncer metastásico.
Factores de riesgo
Existen muchos factores que pueden aumentar el riesgo de carcinoma hepatocelular. Los factores de riesgo más comunes son la cirrosis, que es la formación de cicatrices en el hígado, y una infección por el virus de la hepatitis B o el virus de la hepatitis C. Existen muchas otras afecciones que pueden dañar el hígado y aumentar el riesgo de carcinoma hepatocelular.
Entre los factores de riesgo para el carcinoma hepatocelular se incluyen los siguientes:
- Edad avanzada. El carcinoma hepatocelular es más común en adultos mayores.
- Infección por el virus de la hepatitis B o el virus de la hepatitis C. La infección actual o previa por el virus de la hepatitis B o el virus de la hepatitis C aumenta el riesgo de carcinoma hepatocelular.
- Cirrosis. La cirrosis es una afección progresiva e irreversible que causa la formación de tejido cicatricial en el hígado. Aumenta las posibilidades de presentar carcinoma hepatocelular.
- Ciertas enfermedades hepáticas hereditarias. Algunas enfermedades hepáticas se transmiten de una generación a otra pueden aumentar el riesgo de carcinoma hepatocelular. Los ejemplos incluyen la hemocromatosis y la enfermedad de Wilson.
- Exceso de grasa en el hígado. La enfermedad hepática esteatósica relacionada con la disfunción metabólica, que antes se llamaba enfermedad del hígado graso no alcohólica, ocurre cuando se acumula grasa en el hígado. Las personas con esta afección tienen un riesgo más alto para carcinoma hepatocelular.
- Diabetes. Las personas con esta afección de la glucosa sanguínea tienen más riesgo de padecer carcinoma hepatocelular que quienes no tienen diabetes.
- Obesidad. Las personas con obesidad tienen un riesgo más alto para cirrosis y exceso de grasa en el hígado. Estas afecciones aumentan el riesgo de carcinoma hepatocelular.
- Exposición a aflatoxinas. Las aflatoxinas son venenos producidos por mohos que crecen en cultivos mal almacenados. Los cultivos, como los granos o cereales y los frutos secos, pueden contaminarse con aflatoxinas, que pueden terminar en los alimentos elaborados con estos productos.
- Consumo excesivo de alcohol. Consumir más que una cantidad moderada de alcohol diariamente durante muchos años puede derivar en daño hepático irreversible y aumentar el riesgo de carcinoma hepatocelular.
- Fumar cigarrillos. Las personas que fuman cigarrillos tienen más riesgo de padecer carcinoma hepatocelular.
Complicaciones
El carcinoma hepatocelular puede diseminarse a otras partes del cuerpo. Cuando se disemina, suele ir a los siguientes lugares:
- pulmones,
- ganglios linfáticos del abdomen,
- huesos,
- glándulas suprarrenales,
- cerebro.
El término médico para la diseminación es metastatizar. Cuando este cáncer se disemina, los profesionales de atención médica lo llaman carcinoma hepatocelular metastásico.
Prevención
Reduce tu riesgo de cirrosis
La cirrosis es la formación de cicatrices en el hígado y aumenta el riesgo de carcinoma hepatocelular. Para reducir el riesgo de cirrosis, puedes seguir estos consejos:
- Si bebes alcohol, hazlo con moderación. Si decides beber alcohol, hazlo con moderación. Para los adultos saludables, significa una copa al día en el caso de las mujeres y hasta dos copas al día en el de los hombres.
- Mantén un peso saludable. Si tienes un peso saludable, mantenlo. Si necesitas bajar de peso, pregunta a un profesional de atención médica cómo hacerlo de manera saludable. Come menos calorías y aumenta de a poco la cantidad de ejercicio.
Recibe la vacuna contra la hepatitis B
La infección por el virus de la hepatitis B aumenta el riesgo de carcinoma hepatocelular. Puedes reducir el riesgo de contraer hepatitis B si recibes la vacuna contra la hepatitis B. La vacuna se puede administrar a casi cualquier persona, incluidos bebés, niños, adultos y adultos mayores.
Toma medidas para prevenir la hepatitis C
La infección por el virus de la hepatitis C aumenta el riesgo de carcinoma hepatocelular. No existe ninguna vacuna contra la hepatitis C, pero puedes reducir el riesgo de contraer la infección.
- Conoce el estado de salud de cualquier pareja sexual. No tengas relaciones sexuales sin protección, a menos que estés seguro de que tu pareja no está infectada con hepatitis B, hepatitis C o cualquier otra infección de trasmisión sexual. Si no conoces el estado de salud de tu pareja, usa un preservativo cada vez que tengas relaciones sexuales.
- No uses drogas intravenosas, pero si lo haces, usa una aguja limpia. Reduce el riesgo de contraer hepatitis C al no inyectarte drogas legales o ilegales que puedan venderse en las calles. Pero si esa no es una opción para ti, asegúrate de que las agujas que uses sean estériles y no las compartas. Las agujas contaminadas son una causa común de infección por hepatitis C. Aprovecha los programas de intercambio de jeringuillas de tu comunidad y considera buscar ayuda para superar tu consumo de drogas ilícitas.
- Busca tiendas seguras y limpias cuando quieras un piercing o un tatuaje. Las agujas que no se esterilizan adecuadamente pueden diseminar el virus de la hepatitis C. Antes de ir a que te hagan un piercing o un tatuaje, investiga las tiendas de tu zona y pregunta a los miembros del personal acerca de sus prácticas de seguridad. Si los empleados de una tienda se niegan a responder tus preguntas o no las toman en serio, esa será una señal de que el lugar no es adecuado para ti.
Buscar tratamiento para la infección por hepatitis B o C
Existen tratamientos disponibles para la infección por hepatitis B y por hepatitis C. Las investigaciones demuestran que el tratamiento puede reducir el riesgo de carcinoma hepatocelular.
Pregunta sobre los exámenes de detección para el cáncer de hígado
Para la mayoría de las personas, no se ha demostrado que los exámenes de detección para el cáncer de hígado reduzcan el riesgo de morir por esta enfermedad y, en general, no se recomiendan. Las personas con afecciones que aumentan el riesgo de cáncer de hígado podrían considerar someterse a exámenes de detección. Las personas con riesgo más alto incluyen aquellas que tienen lo siguiente:
- Infección por hepatitis B.
- Infección por hepatitis C.
- Cirrosis de hígado.
Habla sobre las ventajas y las desventajas de los exámenes de detección con tu equipo de atención médica. Juntos pueden decidir si los exámenes de detección son adecuados para ti en función de tu riesgo. Los exámenes de detección para el carcinoma hepatocelular generalmente incluyen un análisis de sangre y una ecografía abdominal cada seis meses.
Dec. 30, 2025