Overview
Shoulder joint
Shoulder joint
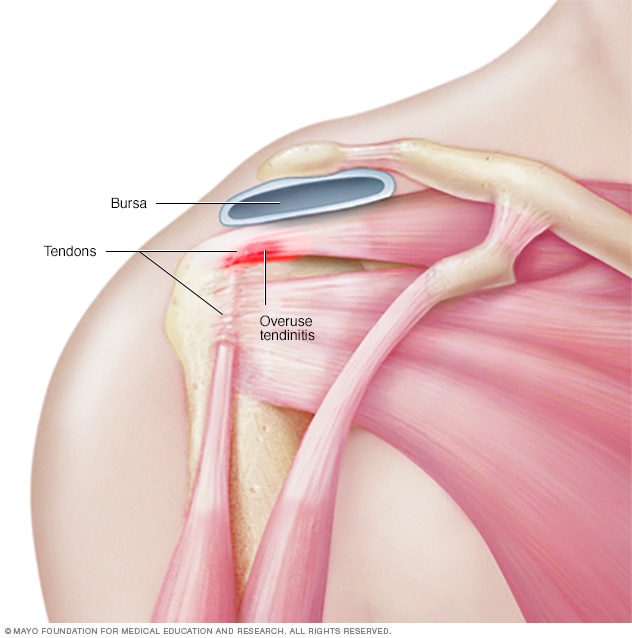
Tendons are thick fibrous cords that attach muscle to bone. Overuse or strain on a joint can inflame tendons and result in tendinitis.
Tendinitis is inflammation of the thick fibrous cords that attach muscle to bone. These cords are called tendons. The condition causes pain and tenderness just outside a joint.
Tendinitis can occur in any tendon. But it's most common around shoulders, elbows, wrists, knees and heels.
Most tendinitis can be treated with rest, physical therapy and medicine to reduce pain. Long-lasting tendon inflammation can cause a tendon to tear. A torn tendon might need surgery.
Products & Services
Types
Symptoms
Symptoms of tendinitis tend to occur where a tendon attaches to a bone. Symptoms often include:
- Pain, often described as a dull ache, especially when moving the hurt limb or joint
- Tenderness
- Mild swelling
When to see a doctor
Most cases of tendinitis respond to self care. See your health care provider if your symptoms don't lessen after a few days and if they get in the way of daily activities.
Causes
Tendinitis can be caused by a sudden injury. But repeating the same movement over time is a much more likely cause. Most people develop tendinitis because their jobs or hobbies involve motions that they repeat, over and over. This puts stress on tendons.
Moving correctly is especially important when having to repeat movements for sports or a job. Moving incorrectly can overload the tendon and lead to tendinitis.
Risk factors
Risk factors for developing tendinitis include age, having jobs that involve doing the same motion over and over, doing physical activities with poor form, and taking certain medicines.
Age
As people get older, their tendons become less flexible — which makes them easier to injure.
Work
Tendinitis is more common in people, such as gardeners and manual laborers, whose jobs involve:
- Repeated motions
- Awkward positions
- A lot of overhead reaching
- Vibration
- Forced movements
Activities
When doing physical activities, the following can increase the risk of tendinitis:
- Sudden increase in amount or difficulty of training
- Poor equipment, such as old shoes
- Hard surfaces, such as concrete or gym floors
- Too little recovery time after an injury or too little time to get used to the activity again after time off
- Poor posture or body movements
Medical condition and medications
Certain medical conditions, such as diabetes, can increase the risk of tendinitis. Medications that may increase risk include:
- Antibiotics known as fluoroquinolines
- Corticosteroids such as cortisone
- Aromatase inhibitors, used to lower breast cancer risk
Complications
Without treatment, tendinitis can increase the risk of a tendon breaking down or tearing. A completely torn tendon might need surgery.
Prevention
To reduce the chance of developing tendinitis, follow these suggestions:
- Ease up. Avoid activities that place too much stress on your tendons, especially for long periods. If you have pain during an exercise, stop and rest.
- Mix it up. If one exercise or activity causes you pain, try something else. Cross-training can help you mix high-impact exercise, such as running, with lower impact exercise, such as biking or swimming.
- Improve the way you move. If how you do an activity or exercise is flawed, you could be setting yourself up for problems with your tendons. Consider taking lessons or getting professional instructions when starting a new sport or using exercise equipment.
- Stretch. After exercise, move your joints through full range of motion. The best time to stretch is after exercise, when your muscles are warmed up.
- Move right in the workplace. Make sure your chair, keyboard and desktop are positioned correctly for your height, arm length and the tasks you do. This will help protect your joints and tendons from stress.
- Prepare your muscles to play. Strengthening muscles used in your activity or sport can help them bear the load better.
Nov. 11, 2022