Diagnosis
To diagnose sleep apnea, your healthcare professional begins by asking about your symptoms and sleep history. Someone who shares your bed or household may be able to provide helpful information.
You're likely to be referred to a sleep center. There, a sleep specialist can recommend further evaluation.
An evaluation often involves overnight monitoring at a sleep center, especially if your healthcare professional suspects that you have CSA. But home sleep testing also might be an option. Tests to detect sleep apnea include:
- Sleep study, also known as polysomnography. During this test, you're hooked up to equipment that monitors your breathing patterns while you sleep. Your heart, lung and brain activity, arm and leg movements, and blood oxygen levels also are measured.
- Home sleep tests. Your healthcare professional might provide you with simplified home tests. These tests usually measure your heart rate, blood oxygen level, airflow and breathing patterns. Since home tests sometimes miss sleep apnea, your healthcare professional might still recommend polysomnography even if your first results are within the standard range.
If you have OSA, your healthcare professional might refer you to an ear, nose and throat doctor to rule out blockage in your nose or throat. You may need to see a heart specialist, known as a cardiologist, or a doctor who specializes in the nervous system, called a neurologist. They can look for causes of central sleep apnea.
Treatment
Continuous positive airway pressure (CPAP)

Continuous positive airway pressure (CPAP)
To eliminate snoring and prevent sleep apnea, a healthcare professional may recommend a device called a continuous positive airway pressure (CPAP) machine. A CPAP machine delivers just enough air pressure to a mask to keep the upper airway passages open, preventing snoring and sleep apnea.
For milder cases of OSA, your healthcare professional may recommend only lifestyle changes, such as losing weight or quitting smoking. You may need to change the position in which you sleep. If you have nasal allergies, your healthcare professional may recommend treatment for your allergies.
If these measures don't improve your symptoms or if your apnea is serious, a number of other treatments are available. Certain devices can help open up a blocked airway. In other cases, surgery might be necessary.
Therapies for OSA
Many people successfully treat OSA with positive airway pressure, also known as PAP, therapies or oral devices. These therapies can prevent stops in breathing and make you more alert during the day.
-
Continuous positive airway pressure, also called CPAP. You might benefit from using a machine that delivers air pressure through a mask while you sleep. With CPAP (SEE-pap), the air pressure is somewhat greater than that of the surrounding air. The greater pressure is just enough to keep your upper airway passages open, preventing apnea and snoring.
Although CPAP is the most common and reliable method of treating sleep apnea, some people find it cumbersome and not comfortable. With practice, most people learn to adjust the tension of the straps on the mask for comfort and to find a secure fit.
You might need to try more than one type of mask to find one with the right fit. Don't stop using the CPAP machine. Check with your healthcare professional to see what changes can be made.
Also contact your healthcare team if you're still snoring or begin snoring again despite treatment. If your weight changes, the pressure settings of the CPAP machine might need to be adjusted.
- Other airway pressure devices. If using a CPAP machine continues to be a problem for you, you might be able to use a different type of airway pressure device that automatically adjusts the pressure while you're sleeping, called auto-CPAP. Devices also can provide more pressure when you inhale and less when you exhale. This is known as bilevel positive airway pressure (BPAP).
-
Oral appliances. Another option is wearing an oral appliance designed to keep your throat open. Typically, CPAP is more effective at opening the airway, but oral appliances might be easier to use. Some are designed to open your throat by bringing your jaw forward, which can sometimes relieve snoring and mild obstructive sleep apnea.
Once you find the right fit, you'll need to follow up with your dentist repeatedly during the first year and then regularly after that. This ensures a good fit.
- Myofunctional therapy. These are exercises that strengthen your upper airway muscles to reduce narrowing of the airway when you sleep. The exercises may be done along with other OSA therapies.
You'll likely read, hear or see TV ads about different treatments for sleep apnea. Don't try a new therapy before talking with your healthcare professional first.
Medicine for OSA
The U.S. Food and Drug Administration has approved the weight loss medicine tirzepatide (Zepbound) to treat obstructive sleep apnea in people with obesity. Clinical trials have found that people who took the medicine had fewer pauses in their breathing and better oxygen levels.
Tirzepatide is an injection taken every week. Side effects can include nausea, diarrhea, vomiting, constipation and stomach pain, among others. The medicine isn't recommended for people who have had medullary thyroid carcinoma or family members who had the disease. It's also not recommended in people with multiple endocrine neoplasia syndrome type 2.
Surgery for OSA
Surgery may be an option for OSA, but usually only if other treatments aren't effective. Generally, at least a three-month trial of other treatment options is suggested before considering surgery. However, for a small number of people with certain jaw structures, it's a good first option.
Surgical options might include:
-
Tissue removal. During this procedure (uvulopalatopharyngoplasty), your healthcare professional removes tissue from the rear of your mouth and top of your throat. Your tonsils and adenoids usually are removed as well.
This type of surgery might be successful in stopping throat structures from vibrating and causing snoring. It's less effective than CPAP and isn't considered a reliable treatment for obstructive sleep apnea.
Removing tissues in the back of your throat with radiofrequency energy (radiofrequency ablation) might be an option if you can't tolerate CPAP or oral appliances.
- Jaw repositioning. In this procedure, your jaw is moved forward from the remainder of your face bones. This enlarges the space behind the tongue and soft palate, making a blockage less likely. This procedure is known as maxillomandibular advancement.
- Nerve stimulation. A device implanted in your chest triggers the nerve involved in tongue movement, known as the hypoglossal nerve. The increased stimulation helps keep the tongue in a position that keeps the airway open. This treatment is used if nonsurgical treatments for OSA haven't worked.
- Creating a new air passageway, known as tracheostomy. You may need this form of surgery if other treatments have failed and you have severe, life-threatening sleep apnea. In this procedure, your surgeon makes an opening in your neck and inserts a metal or plastic tube through which you breathe. You keep the opening covered during the day. But at night you uncover it to allow air to pass in and out of your lungs, bypassing the blocked air passage in your throat.
Other types of surgery may help reduce snoring and contribute to the treatment of sleep apnea by clearing or enlarging air passages:
- Weight-loss surgery, also known as bariatric surgery.
Therapies for CSA
If you have CSA, your healthcare professional may recommend one of these therapies.
- Treatment for related medical problems. Possible causes of central sleep apnea include heart or neuromuscular disorders, and treating those conditions might help.
- PAP devices. Your healthcare professional may recommend CPAP or BPAP devices. A more recently approved airflow device is called adaptive servo-ventilation (ASV), also known as ASV. It learns your typical breathing pattern and stores the information in a built-in computer. After you fall asleep, the machine uses pressure to regulate your breathing pattern and prevent pauses in your breathing. ASV may be an option for some people with treatment-emergent central sleep apnea. However, ASV is not recommended for those with severe heart failure.
- Supplemental oxygen. Using supplemental oxygen while you sleep might help if you have CSA.
- Medicine changes. You may be prescribed medicine to help manage your breathing, such as acetazolamide. If medicines are worsening your CSA, such as opioids, your healthcare professional may change your medicines.
- Transvenous phrenic nerve stimulation. During this treatment, your healthcare professional implants a stimulator in your chest. The system affects the nerve involved in your breathing, known as your phrenic nerve. If the system detects that your breathing has stopped, it triggers the nerve to help you breathe.
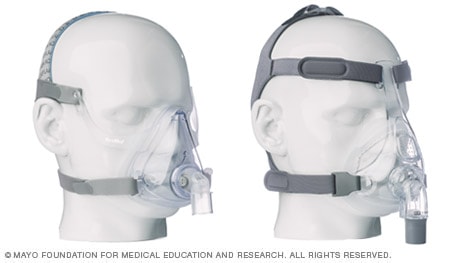
Many CPAP mask options available
Continuous positive airway pressure (CPAP) masks and headgear come in many styles and sizes to comfortably treat your sleep apnea. Everyone has different needs, preferences and face shapes, and sometimes you will need to try different mask styles before you find the one that works the best for you.
Sizes may vary across different mask styles and brands. You may need to try on several styles and sizes to find the best combination of comfort and efficiency.
For example, if you take a small in one type it does not necessarily mean you will need a small in a different brand. Proper sizing is very important to comfort and performance of masks.
Here's a look at a few CPAP mask styles and some possible benefits of each. Work with your doctor and CPAP mask supplier to make sure you have a mask that suits your needs and fits you properly.
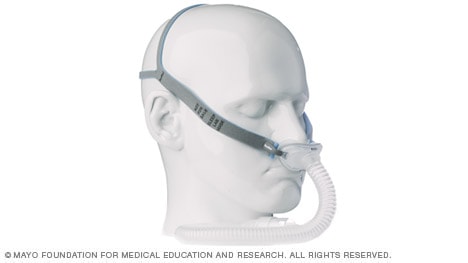
Nasal pillow mask
Nasal pillows fit at the nares to supply air pressure.
Might be good if:
- You feel claustrophobic in masks that cover more of your face
- You want a full field of vision for reading or watching TV
- You want to wear your glasses
- You have facial hair that interferes with other masks
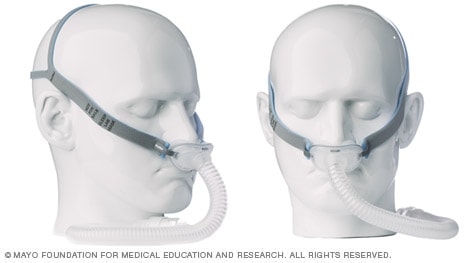
Nasal masks
The mask covering the nose supplies air pressure.
Might be good if:
- Your doctor has prescribed a high air pressure setting
- You move around a lot in your sleep
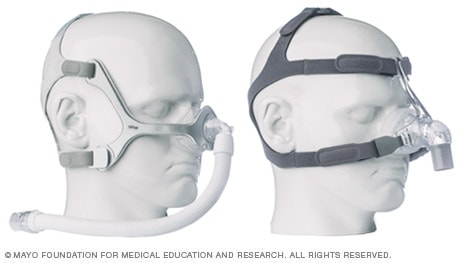
Full-face masks
The mask covering the nose and mouth supplies air pressure.
Might be good if:
- You have nasal obstruction or congestion that makes breathing through your nose difficult
- You breathe through your mouth at night despite a month of trying a nasal mask or nasal pillow interface combined with a heated humidity feature or chin strap or both to keep your mouth closed
More Information
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
Self-care might be a way for you to deal with obstructive sleep apnea and possibly central sleep apnea. Try these tips:
- Lose excess weight. Even a slight weight loss might help relieve constriction of your throat. In some cases, sleep apnea can resolve if you return to a healthy weight, but it can recur if you regain the weight.
- Exercise. Regular exercise can help ease the symptoms of obstructive sleep apnea even without weight loss. Try to get 30 minutes of moderate activity, such as a brisk walk, most days of the week.
- Avoid alcohol and certain medications, such as sleeping pills. These relax the muscles in the back of your throat, interfering with breathing.
- Sleep on your side or stomach rather than on your back. Sleeping on your back can cause your tongue and soft palate to rest against the back of your throat and block your airway. To keep from rolling onto your back while you sleep, try attaching a tennis ball to the back of your pajama top. There also are commercial devices that vibrate when you roll onto your back in sleep.
- Don't smoke. If you're a smoker, look for resources to help you quit.
Preparing for your appointment
If you or your partner suspects that you have sleep apnea, contact your healthcare professional. You might be referred right away to a sleep specialist.
Here's some information to help you get ready for your appointment.
What you can do
When you make the appointment, ask if there's anything you need to do in advance, such as modify your diet or keep a sleep diary.
Make a list of:
- Your symptoms, including any that may seem unrelated to the reason for which you scheduled the appointment, and when they began.
- Key personal information, including family history of a sleep condition.
- All medicines, vitamins or supplements you take, including doses.
- Questions to ask your healthcare professional.
Take a family member or friend along, if possible, to help you remember the information you receive. Because your bed partner might be more aware of your symptoms than you are, it may help to have him or her along.
For sleep apnea, some questions to ask your healthcare professional include:
- What's the most likely cause of my symptoms?
- What tests do I need? Do these tests require special preparation?
- Is my condition likely short term or long lasting?
- What treatments are available?
- Which treatment do you think would be best for me?
- I have other health conditions. How can I best manage these conditions together?
- Should I see a specialist?
- Are there brochures or other printed material that I can have? What websites do you recommend?
What to expect from your doctor
Your healthcare professional is likely to ask you questions, including:
- Have your symptoms been constant, or do they come and go?
- How severe are your symptoms?
- How does your partner describe your symptoms?
- Do you know if you stop breathing during sleep? If so, how many times a night?
- Is there anything that has helped your symptoms?
- Does anything make your symptoms worse, such as sleep position or alcohol consumption?
What you can do in the meantime
- Try to sleep on your side.
- Avoid alcohol for 4 to 6 hours before bed.
- Don't take medicines that make you sleepy.
- If you're drowsy, avoid driving.
Dec. 09, 2025