Jan. 07, 2026
The incidence of obesity-related liver disease, also known as metabolic dysfunction-associated steatotic liver disease (MASLD), has mirrored the increase in the incidence of obesity. MASLD is now the most common type of liver disease in the United States and worldwide.
"MASLD and hepatocellular carcinoma secondary to MASLD also are now among the most common reasons for liver transplantation referral," explains Julie K. Heimbach, M.D., a transplant surgeon and researcher at Mayo Clinic William J. von Liebig Center for Transplantation and Clinical Regeneration in Rochester, Minnesota. "However, the optimal approach to managing patients with both obesity and advanced liver disease is still unclear."
Bariatric surgery is one strategy employed to manage the burden of obesity and comorbid conditions, including metabolic syndrome (MetS), that affect transplant candidates with class 3 obesity. Bariatric surgery can be performed before, during or after liver transplantation (LT). However, researchers are still working to determine the most advantageous timing and sequencing for these surgeries.
Bariatric surgeries performed before and after LT are associated with some well-documented challenges. Elective surgery in patients with decompensated cirrhosis is associated with higher perioperative mortality rates. Consequently, bariatric surgeries performed before LT are typically recommended only for patients with very early stages of liver disease. These are typically not patients who need to undergo transplant. Bariatric surgeries performed after LT can be more technically challenging because of the presence of adhesions and altered anatomy, and the risks of long-term immunosuppression.
Sleeve gastrectomy
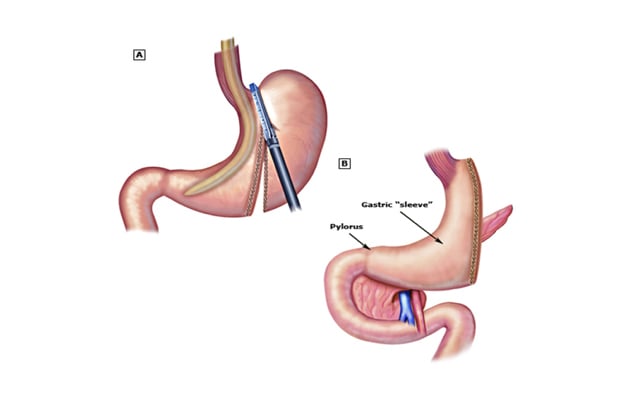
Sleeve gastrectomy
A: Stapling of the greater curvature of the stomach in sleeve gastrectomy. B: Completed sleeve gastrectomy.
Performing these two surgeries simultaneously to treat both liver failure (with LT) and obesity (with sleeve gastrectomy) has emerged as another approach. Although case reports and single-center series have yielded some promising outcomes, more data is needed to demonstrate that the simultaneous surgery approach is safe and that it provides long-term benefits.
To address these knowledge gaps, Dr. Heimbach and researchers from Mayo Clinic campuses in Minnesota, Arizona and Florida conducted the first multicenter study analyzing the long-term impact of providing simultaneous liver transplant and sleeve gastrectomy (LTSG) for patients with obesity and MASLD. The results of this study were published in the Journal of Hepatology in 2025, with Dr. Heimbach serving as the corresponding author.
Methods
In a multicenter, retrospective cohort study, Mayo Clinic researchers analyzed and compared the long-term outcomes from two groups of patients.
Patient cohorts:
- LTSG group of 72 patients with decompensated liver disease and a mean baseline body mass index (BMI) of 45.5 underwent simultaneous LTSG.
- LT alone group of 185 patients with MASLD and a mean baseline BMI of 34 underwent LT for MASLD.
After following the simultaneous LTSG group for 4 to 153 months and the LT alone group for 12 to 161 months, the researchers documented multiple outcomes. The outcome analysis compared rates of mortality, graft loss, BMI, metabolic syndrome components, allograft steatosis and fibrosis, and gastroesophageal reflux, which is a well-documented long-term complication of sleeve gastrectomy.
Results
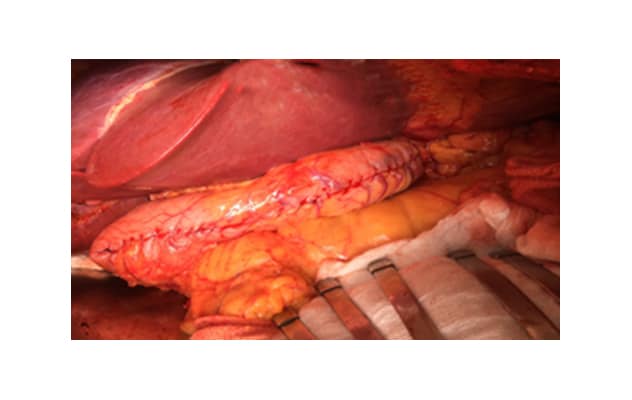 Simultaneous surgery
Simultaneous surgery
A successful simultaneous liver transplant and sleeve gastrectomy.
"Overall, the study results established that simultaneous liver transplant plus sleeve gastrectomy is effective in providing long-term treatment of both end-stage liver disease and metabolic syndrome, including obesity, diabetes mellitus, steatosis and potentially fibrosis," explains Dr. Heimbach.
Researchers observed multiple benefits associated with simultaneous LTSG versus LT alone, including the following:
- The LTSG group experienced significant, sustained weight loss for at least nine years after surgery when compared with baseline BMI. No significant change was observed in the LT alone group.
- The prevalence of postoperative diabetes was significantly lower in the LTSG group than in the LT alone group. This difference persisted for at least eight years after surgery.
- The prevalence of hypertension decreased significantly after surgery in the LTSG group.
- The incidence of allograft steatosis was significantly lower in the LTSG group compared with the LT alone group.
- The prevalence of fibrosis at 3 to 10 years after surgery was lower in the LTSG group compared with the LT alone group.
- Severe gastroesophageal reflux disease occurred in 11.1% of the LTSG group.
- The LTSG and LT alone groups experienced comparable rates of mortality, graft loss and major cardiovascular events.
Next steps
Dr. Heimbach notes that additional studies are needed to focus on the optimal timing for bariatric surgery — simultaneous versus staged — and to determine the cost-effectiveness of and most appropriate role for glucagon-like peptide-1 (GLP-1) agonists and other medical treatments.
For more information
Larson EL, et al. Simultaneous liver transplant and sleeve gastrectomy provides durable weight loss, improves metabolic syndrome and reduces allograft steatosis. Journal of Hepatology. 2025;83:729.
Refer a patient to Mayo Clinic.