Jan. 25, 2022
Abdominal pain is one of the most common gastrointestinal (GI) problems causing individuals to seek medical care within the United States. Functional GI disorders, also known as disorders of gut-brain interaction (DGBI), are common underlying causes of abdominal pain in many patients. This highly prevalent category of GI disorders includes irritable bowel syndrome (IBS), functional dyspepsia (FD) and centrally mediated abdominal pain syndrome (CAPS).
Clinicians frequently prescribe antispasmodic agents to treat symptoms of abdominal pain, including spasms and cramps, in patients with DGBI. Within the U.S., the number of prescriptions for these medications is estimated to exceed 3 million a year.
Antispasmodics available in North America
Antispasmodics available in North America
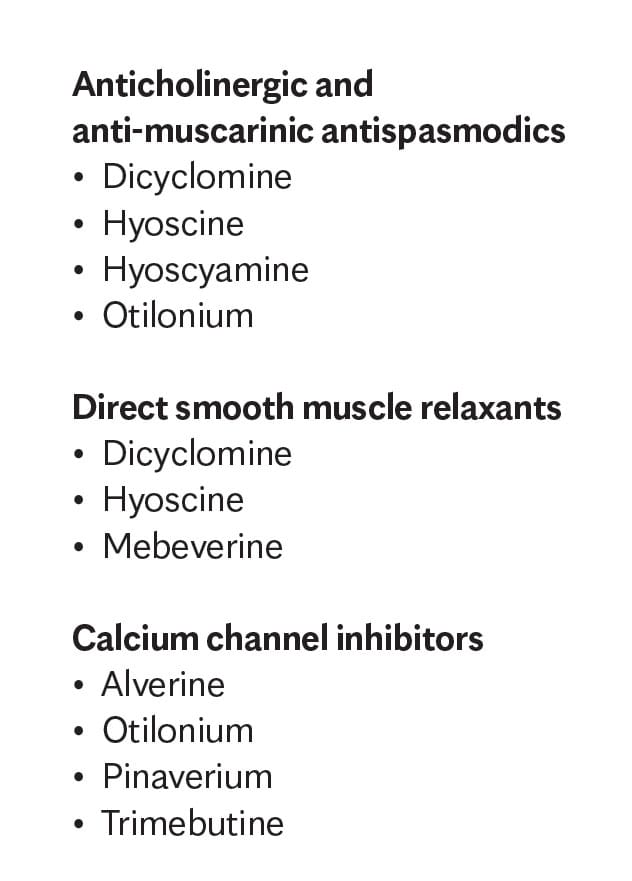
Currently, three categories of antispasmodics are available in North America, each of which has a different mechanism of action.
In a review article published in The American Journal of Gastroenterology in 2021, co-authors Darren M. Brenner, M.D., and Brian E. Lacy, M.D., Ph.D., examine the published data related to the use of antispasmodic agents available in North America for the treatment of abdominal pain in patients with DGBI. Dr. Lacy is a gastroenterologist at Mayo Clinic in Jacksonville, Florida, and a co-author of the American College of Gastroenterology (ACG) clinical guideline for the management of IBS published in 2021.
Currently, three categories of antispasmodics are available in North America, each of which has a different mechanism of action:
- Anticholinergic and anti-muscarinic agents, which inhibit GI smooth muscle contraction
- Calcium channel inhibitors, which inhibit calcium transport into GI smooth muscle
- Direct smooth muscle relaxants, which inhibit sodium and calcium transport
Methods
Seeking to examine the efficacy and safety of these medications more closely, the co-authors conducted a review of available randomized, placebo-controlled, parallel or crossover studies of antispasmodics currently available in North America (United States, Canada and Mexico) that involved adults with abdominal pain related to IBS, dyspepsia or FD, and CAPS.
The co-authors' database search identified a total of 26 studies, including 23 focused on IBS, one on FD and two on recurrent abdominal pain with cramping. The search did not identify any studies evaluating antispasmodics in patients with CAPS. The co-authors then analyzed each study's patient population, treatment regimen, efficacy outcomes and safety outcomes.
Discussion and results
The co-authors provide detailed information and charts summarizing the available data related to each of the specific medications that are currently available in North America for the treatment of chronic abdominal pain related to DGBI. After performing this analysis, Drs. Lacy and Brennan concluded that data supporting the use of antispasmodics for the treatment of chronic abdominal pain in patients with DGBI, including IBS and FD, are limited. They note that many of the trials included in this analysis have limited sample size, short duration of therapy, heterogeneity in outcomes and concerns related to study design bias.
"The antispasmodics studied were found to vary dramatically in efficacy and safety. This makes it difficult to recommend these agents for clinical use, especially after comparing the data sets available from large, randomized, controlled trials evaluating the performance of IBS medications currently approved for use in the United States," explains Dr. Lacy.
"Our research also highlights the need to use other approved therapies to treat chronic abdominal pain, such as neuromodulators and cognitive behavioral therapy, and to engage in additional research to develop and test agents to treat this debilitating disorder," says Dr. Lacy. Researchers at Mayo Clinic in Jacksonville, Florida, are evaluating the use of virtual reality to treat abdominal pain symptoms in patients with functional dyspepsia. Preliminary results were shared at the 2021 meeting of the American College of Gastroenterology in Las Vegas.
For more information
Brenner DM, et al. Antispasmodics for chronic abdominal pain: Analysis of North American treatment options. The American Journal of Gastroenterology. 2021;116:1587.
Lacy BE, et al. ACG clinical guideline: Management of irritable bowel syndrome. The American Journal of Gastroenterology. 2021;116:17.
Refer a patient to Mayo Clinic.