May 25, 2018
Graves' orbitopathy (GO) — also known as Graves' ophthalmopathy, thyroid-associated orbitopathy and thyroid eye disease — is an entity that requires multispecialty evaluation with involvement of endocrinologists, ophthalmologists and ENT surgeons for optimal management.
Marius N. Stan, M.D., with Endocrinology, Diabetes, Metabolism, & Nutrition at Mayo Clinic's campus in Rochester, Minnesota, explains: "Timing these evaluations closely together can be a challenge, as patients typically call in to schedule with only one provider. Given the expected fluctuations in the disease, having the evaluations scattered over weeks to months does not allow for a seamless collaboration between these physicians.
"This issue has been tackled by the European Group on Graves' Orbitopathy (EUGOGO) and led to the establishment of multispecialty clinics dedicated to GO, where the patients are seen by both an endocrinologist and an ophthalmologist. A joint assessment is then made and an agreed upon management plan is devised.
Algorithm for assessing severity of Graves' orbitopathy
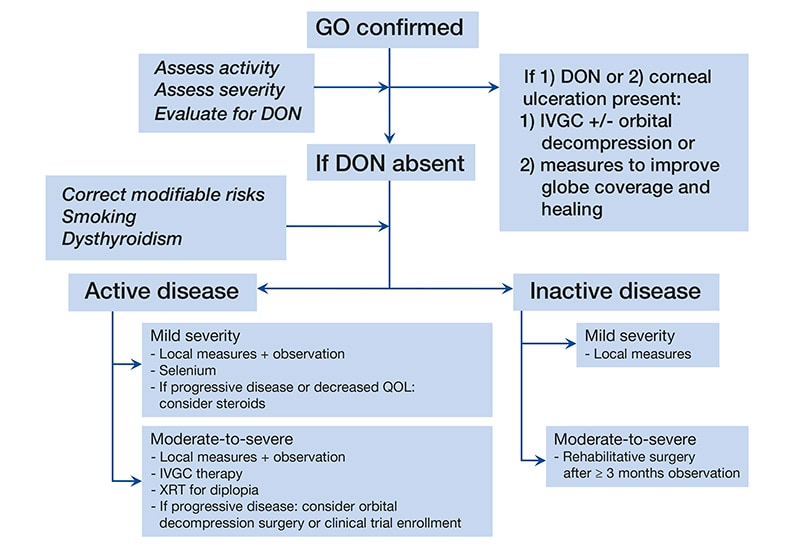
Algorithm for assessing severity of Graves' orbitopathy
Algorithm for assessing severity of Graves' orbitopathy and treatment options. Abbreviations used: DON, dysthyroid optic neuropathy; GO, Graves' orbitopathy; IVGC, intravenous glucocorticoid; and, XRT, external beam radiation therapy.
"We have expanded from that practice here at Mayo Clinic with the inclusion of an ENT surgeon and have created a clinic where the three specialties converge. Their individual evaluations are combined into one summary assessment and management plan. The patients are seen in the morning in individual consultations by each of the three physicians involved. They are then discussed at a noon conference where patients' photographs and laboratory data are reviewed. We assess disease activity, severity and modifiable risk factors. A common plan of action is agreed upon and that is presented to the patient in a brief follow-up visit that same afternoon by the ophthalmologist and the endocrinologist."
Elizabeth A. Bradley, M.D., an ophthalmologist at Mayo Clinic's Minnesota campus, notes: "The ophthalmologic evaluation includes an assessment of the visual acuity, color vision, visual field and ocular motility. Patients also undergo a comprehensive examination of the eye, including the conjunctiva, cornea, optic nerve and retina. The external examination includes quantitative assessment of upper and lower eyelid position and exophthalmometry."
Anatomic relationships of a medial wall orbital decompression
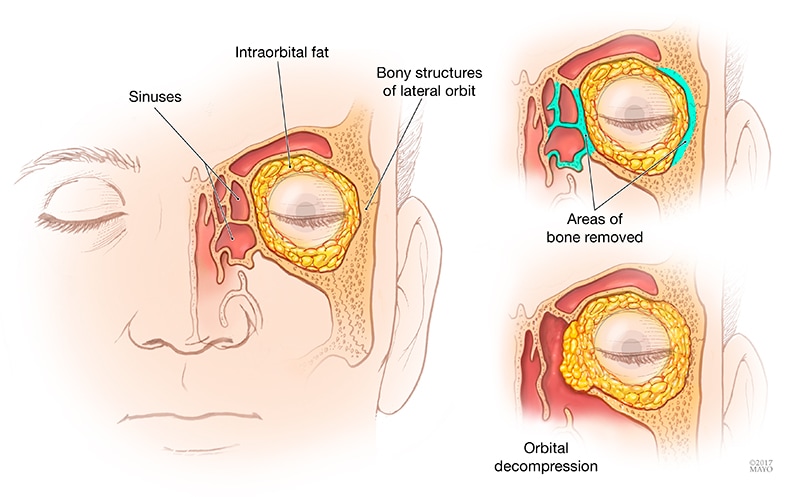
Anatomic relationships of a medial wall orbital decompression
Anatomic relationships of a medial wall orbital decompression, which can be performed in isolation or in combination with a lateral orbital decompression for moderate and severe disease.
Janalee K. Stokken, M.D., an otorhinolaryngologist at Mayo Clinic's Minnesota campus, says: "I focus on discussing and performing endoscopic medial wall orbital decompressions when deemed necessary. This is a surgical procedure that can be performed in isolation or in combination with a lateral orbital decompression in conjunction with ophthalmology for moderate and severe disease. The main goal is to address significant proptosis or corneal exposure, optic neuropathy and, occasionally, persistent retro-orbital pain despite other therapies.
"The medial wall decompression is performed in a minimally invasive fashion utilizing endoscopic techniques similar to sinus surgery that avoids incisions in the mouth or on the face. Another benefit of the endoscopic approach is the ability to open the sinus cavities that can become obstructed from the decompression."
Erick D. Bothun, M.D., a surgical ophthalmologist at Mayo Clinic's Minnesota campus, shares: "Throughout patients' disease course, they are evaluated by both an orbital surgeon and a strabismus (eye muscle) surgeon. The surgical teams discuss and tailor the approach for each individual patient to minimize or eliminate postoperative eye misalignment and double vision."
Dr. Stan adds: "From the endocrine perspective, we assess the patients' thyroid status, risk factors for GO progression, and the activity and severity of GO itself. We aim to restore euthyroidism expeditiously and, when needed, engage the support of our nicotine dependence counseling team.
"We classify GO activity using the clinical activity score and the severity based on EUGOGO guidelines with the categories of mild, moderate to severe, and sight threatening. If active GO is identified, anti-inflammatory and immunomodulatory therapy are discussed and the risks and benefits of such therapies are outlined."
Dr. Stan highlights: "We conduct the clinic on a monthly basis. Patients have orthoptics, thyroid function tests, a TSH receptor antibody test and an orbital CT prescheduled for the same day. The latter is set for the afternoon, in the event surgical intervention is not planned. We also utilize the services of our Infusion Therapy Center; when the treatment is considered necessary, the first dose of intravenous methylprednisolone is administered the same day.
"We see the clinic as an effective way to have a multidisciplinary evaluation for GO patients with GO in a timely manner that allows rapid decision-making and agreement between the specialties involved in the sequence of steps to be followed. We also see the educational benefit both for staff and for trainees with this challenging entity that is still in need of therapeutic improvements.
"We plan to expand this approach to a bimonthly schedule as well as expand the numbers of providers involved to facilitate that increase. The clinic will be tied to our ongoing and future research protocols, offering patients access to potential new diagnostic and therapeutic advances."