May 29, 2015
Primary hyperparathyroidism (HPT) is the most common cause of hypercalcemia, affecting as many as 1 in 750 people and 1 in 500 women over the age of 60 years.
Geoffrey B. Thompson, M.D., at Mayo Clinic's campus in Rochester, Minnesota, says: "For many years, standard bilateral cervical exploration was the gold standard, with a cure rate higher than 98 percent and risk of recurrent laryngeal nerve damage or hypoparathyroidism of less than 1 percent. However, bilateral exploration generally requires a larger incision and involves operative exploration of both sides of the central neck, thereby potentially engendering risk to recurrent laryngeal nerves as well as all four parathyroid glands.
Incision reveals lower poles of thyroid lobes
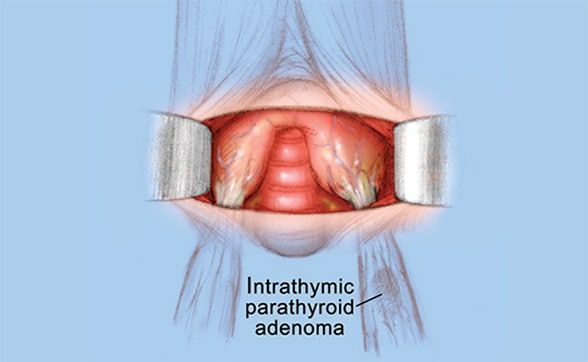
Incision reveals lower poles of thyroid lobes
Through this small incision, the lower poles of each thyroid lobe are seen.
Elevated lobe reveals parathyroid adenoma
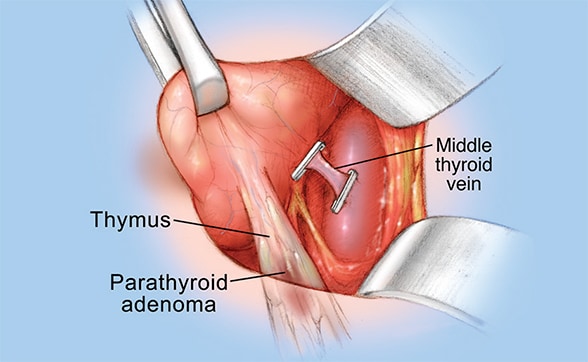
Elevated lobe reveals parathyroid adenoma
The lower pole of the left thyroid lobe is elevated, and a small venous branch is clipped and cut. The parathyroid adenoma is seen, somewhat hidden in the portion of the thymus attached to the thyroid.
Closed incision
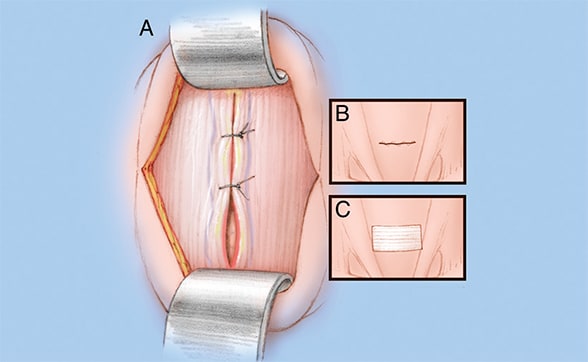
Closed incision
After the parathyroid adenoma has been removed, the incision is closed by suturing the muscles (A) and skin (B) with internal dissolvable sutures, and a small bandage is applied (C).
Locally anesthetized site
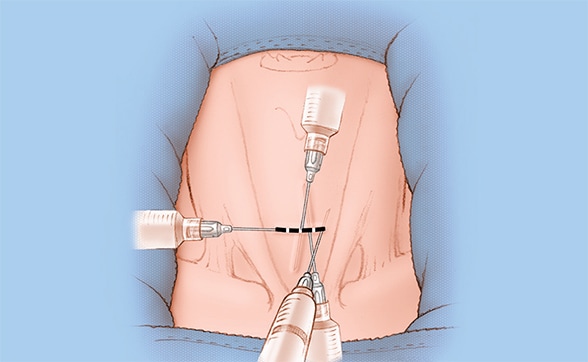
Locally anesthetized site
The small, 3-cm incision site is locally anesthetized.
"With the introduction of several key advances, this highly successful operation has been further refined with patient-focused improvements that have prompted a shift from the standard bilateral surgical approach to a more focused operation."
Focused parathyroidectomy entails an image-guided exploration of a single parathyroid adenoma with the utilization of intraoperative parathyroid hormone (PTH) monitoring to define a biochemical cure.
Focused parathyroidectomy has emerged as a popular technique in endocrine surgery. Key advances that have facilitated the development of focused parathyroidectomy are threefold:
- High-quality parathyroid adenoma localization techniques
- Highly accurate rapid intraoperative PTH monitoring
- The ability to carry out these operations through smaller incisions, often resulting in earlier hospital dismissal and return to usual activities
High-quality localization techniques
Melanie L. Richards, M.D., at Mayo Clinic's campus in Minnesota, says: "Considerable improvements in and widespread use of sophisticated and accurate imaging modalities have allowed for preoperative localization of a single parathyroid adenoma in the majority of patients with primary HPT.
"Preoperative localization allows for the focused exploration and resection of the single offending gland without the need for bilateral four-gland exploration. Frequently utilized imaging modalities include parathyroid technetium-sestamibi (MIBI) scintigraphy, ultrasonography and 4-D computerized tomography (4D-CT).
"Dual isotope subtraction MIBI scanning with the utilization of single-photon emission computerized tomography (SPECT) and CT fusion has become the localization procedure of choice at Mayo Clinic. It is minimally invasive and depends on physiologic hyperfunction of the enlarged parathyroid gland rather than on purely anatomic identification. Adenomas anywhere in the neck or mediastinum can be localized with the addition of SPECT and CT fusion images.
"MIBI scanning is somewhat less dependent than cervical ultrasonography on the size of the parathyroid adenoma for imaging, but the cost is usually higher. A major advantage of MIBI scanning over ultrasonography is that it is less dependent on operator experience to obtain a high-quality scan. The sensitivity of MIBI scanning is 75 to 88 percent."
Travis J. McKenzie, M.D., a surgeon at Mayo Clinic's campus in Minnesota, adds: "High-resolution parathyroid ultrasonography has gained popularity in recent years. It is noninvasive and the most inexpensive preoperative localization technique. Unlike parathyroid scintigraphy and CT, there is no radiation exposure to the patient.
"Ultrasound is anatomically precise and capable of identifying 95 percent of adenomas weighing more than 1,000 mg. However, ultrasonography identifies less than 50 percent of adenomas weighing less than 200 mg. Its sensitivity and specificity are approximately 60 percent and 90 percent, respectively.
"Ultrasound carries the added advantage of concomitantly identifying thyroid pathology. The key limiting factor for ultrasonographic localization is its dependence on a skilled operator. Furthermore, ectopic glands located in the mediastinum or tracheoesophageal groove are not readily identifiable with ultrasound, and adenomas may be obscured in the setting of nodular thyroid disease.
"A newer imaging modality, 4D-CT employs multiphase contrast-enhanced CT imaging relying on the early arterial contrast enhancement and washout to identify parathyroid glands. This technique provides highly accurate anatomic detail that a clinician can readily interpret. In addition, 4D-CT has been demonstrated to be > 90 percent accurate in identifying single adenomas, with an overall sensitivity ranging from 70 to 90 percent.
"Furthermore, this modality provides excellent anatomic imaging of the tracheoesophageal groove and retroesophageal ectopic glands as well as the mediastinum. However, 4D-CT is costly and results in radiation exposure."
High-quality, rapid intraoperative PTH measurement
David R. Farley, M.D., at Mayo Clinic's campus in Minnesota, says: "Intraoperative PTH monitoring has a turnaround time of approximately 30 minutes or less and can therefore be utilized in the operating room to confirm resection of the offending parathyroid adenoma by demonstrating a rapid decline in PTH levels. This allows for highly accurate confirmation of surgical cure without the need for four-gland cervical exploration in patients with single adenomas. The accuracy of intraoperative PTH measurement has been widely verified and enthusiastically supported. Cost ranges from $350 to $750 a patient."
Small-incision outpatient procedure
The option of local anesthesia, a small incision and brief outpatient recovery time are further advantages of the unilateral focused approach.
The Mayo Clinic experience
Dr. Thompson explains: "In June 1998, we introduced focused parathyroidectomy at Mayo Clinic. Through September 2009, we performed 3,203 parathyroid operations. During recent years, 75 percent of patients had the focused procedure. Ninety-seven percent of patients who required a standard four-gland exploration had specific contraindications for the focused approach. The cure rate for both conventional open exploration and focused parathyroidectomy was 97 percent."
Dr. Richards highlights: "Localization was performed with MIBI scanning and ultrasonography in the majority of cases. The sensitivity and positive predictive value of MIBI were 86 percent and 92 percent, respectively; comparable figures for ultrasonography were 62 percent and 90 percent, respectively.
"Important to these figures is the median weight of the largest resected parathyroid gland of 430 mg and a mean calcium value of 11.0 mg/dL (normal, 8.9 to 10.1 mg/dL). Intraoperative PTH monitoring was associated with a sensitivity, positive predictive value, and accuracy of 98 percent, 99 percent, and 97 percent, respectively. The true negative rate, defined as no decline in the PTH value when the patient still had an additional enlarged parathyroid gland, was 8 percent."
Dr. McKenzie notes: "Of the patients undergoing focused parathyroidectomy, 70 percent received general anesthesia, and 30 percent had a combination of local anesthesia and intravenous sedation. Changes in anesthetic technique have allowed our patients undergoing general anesthesia to be discharged from the hospital early with much less nausea.
"Correspondingly, 89 percent of our patients were dismissed from the hospital as outpatients, whereas 11 percent were hospitalized, most often due to comorbidities necessitating in-hospital observation."
Dr. Farley concludes: "The successful outcome of parathyroid surgery, specifically focused parathyroid exploration, depends on a centralized, highly skilled, experienced multidisciplinary team to achieve consistently successful outcomes."