Overview
Female reproductive system
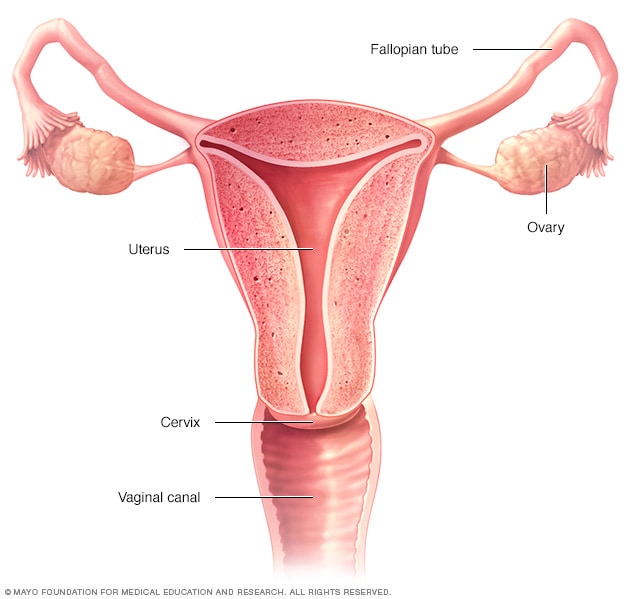
Female reproductive system
The ovaries, fallopian tubes, uterus, cervix and vagina, also called the vaginal canal, make up the female reproductive system.
Cervicitis is an inflammation of the cervix, the lower, narrow end of the uterus that opens into the vagina.
Possible symptoms of cervicitis include bleeding between menstrual periods, pain with intercourse or during a pelvic exam, and abnormal vaginal discharge. However, it's also possible to have cervicitis and not experience any signs or symptoms.
Often, cervicitis results from a sexually transmitted infection, such as chlamydia or gonorrhea. Cervicitis can develop from noninfectious causes, too. Successful treatment of cervicitis involves treating the underlying cause of the inflammation.
Products & Services
Symptoms
Cervicitis
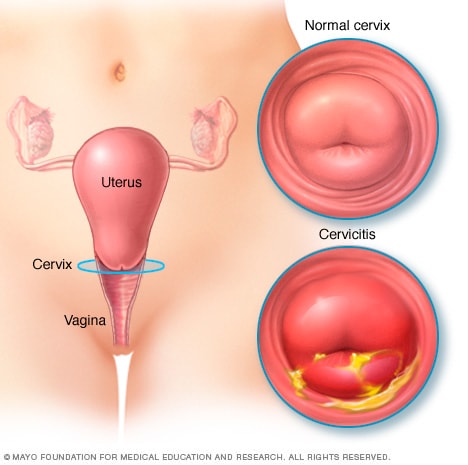
Cervicitis
With cervicitis, an inflammation of your cervix, your cervix appears red and irritated and may produce a pus-like discharge.
Most often, cervicitis causes no signs and symptoms, and you may only learn you have the condition after a pelvic exam performed by your doctor for another reason. If you do have signs and symptoms, they may include:
- Large amounts of unusual vaginal discharge
- Frequent, painful urination
- Pain during sex
- Bleeding between menstrual periods
- Vaginal bleeding after sex, not associated with a menstrual period
When to see a doctor
See your doctor if you have:
- Persistent, unusual vaginal discharge
- Nonmenstrual vaginal bleeding
- Pain during sex
Causes
Possible causes of cervicitis include:
- Sexually transmitted infections. Most often, the bacterial and viral infections that cause cervicitis are transmitted by sexual contact. Cervicitis can result from common sexually transmitted infections (STIs), including gonorrhea, chlamydia, trichomoniasis and genital herpes.
- Allergic reactions. An allergy, either to contraceptive spermicides or to latex in condoms, may lead to cervicitis. A reaction to feminine hygiene products, such as douches or feminine deodorants, also can cause cervicitis.
- Bacterial overgrowth. An overgrowth of some of the bacteria that are normally present in the vagina (bacterial vaginosis) can lead to cervicitis.
Risk factors
You're at greater risk of cervicitis if you:
- Engage in high-risk sexual behavior, such as unprotected sex, sex with multiple partners or sex with someone who engages in high-risk behaviors
- Began having sexual intercourse at an early age
- Have a history of sexually transmitted infections
Complications
Your cervix acts as a barrier to keep bacteria and viruses from entering your uterus. When the cervix is infected, there's an increased risk that the infection will travel into your uterus.
Cervicitis that's caused by gonorrhea or chlamydia can spread to the uterine lining and the fallopian tubes, resulting in pelvic inflammatory disease (PID), an infection of the female reproductive organs that can cause fertility problems if left untreated.
Cervicitis can also increase the risk of getting HIV from an infected sexual partner.
Prevention
To reduce your risk of cervicitis from sexually transmitted infections, use condoms consistently and correctly each time you have sex. Condoms are very effective against the spread of STIs, such as gonorrhea and chlamydia, which can lead to cervicitis. Being in a long-term relationship in which both you and your uninfected partner are committed to having sex with each other exclusively can lower your odds of an STI.
Jan. 31, 2023