July 27, 2022
Chronic and progressive, glaucomatous optic neuropathy (GON) results in characteristic cupping of the optic nerve and visual field loss. GON accounts for more than 8% of blindness worldwide.
The most significant risk factor for the development of GON is intraocular pressure (IOP). Ocular hypertension (OHTN) — the presence of elevated IOP without evidence of GON — is also a risk factor for development.
"The only reliable treatment for GON is lowering IOP with medications, laser or surgery. Yet even when successful, these treatments may only delay progression, with side effects and repeated dosing leading to compliance issues and high economic burden," says Gavin W. Roddy, M.D., Ph.D., an ophthalmologist at Mayo Clinic in Rochester, Minnesota. "Lifestyle factors, however, may impact the development of glaucoma, so the prevention or reduction of progression risk through lifestyle modification is an attractive low-risk, high-reward intervention."
Dr. Roddy notes: "Defining a person's overall state of health related to lifestyle is challenging. There are many variables, including underlying genetic predisposition, diet and exercise. Metabolic syndrome (MetS) is a definable endpoint, yet knowledge gaps exist in our understanding of the association of MetS with GON and OHTN."
Multiple mechanisms of disease are common between MetS and GON and some prior studies suggested an association among MetS and OHTN and GON. However, prior studies left unclear:
- Whether studies performed in other patient populations, including those of East Asian descent, could be readily applied to patients in the United States who are more likely to consume a Western diet, which is a significant risk factor for MetS
- The contribution of central corneal thickness (CCT), which not only can influence the measurement of IOP but also is an independent risk factor for the development of GON
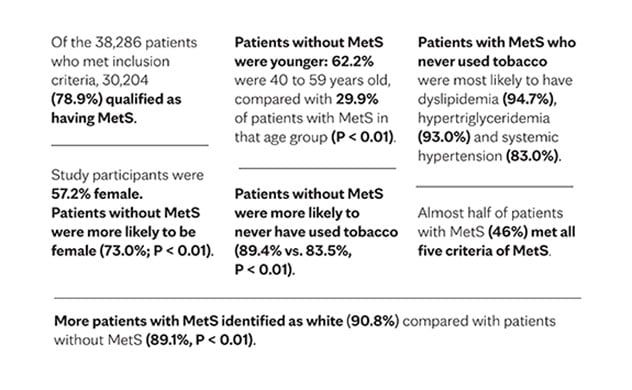
To address those knowledge gaps, Dr. Roddy and fellow researchers conducted a retrospective chart review using the Rochester Epidemiology Project, a collaboration of health care providers in Olmsted County, Minnesota, that shares patient medical records, with permission, to researchers. Their findings were published in the Journal of Glaucoma in 2021.
Patient identification
Patients were identified as having MetS based on diagnosis codes, laboratory values and medication use, or if they met at least three of the following five previously established criteria:
- Body mass index 27 kg/m2 or higher, substituted for waist circumference
- Triglycerides greater than or equal to 150 mg/dL, or treatment for or diagnosis of hypertriglyceridemia
- HDL-C less than 40 mg/dL in men, HDL-C less than 50 mg/dL in women, or treatment for or diagnosis of dyslipidemia
- Blood pressure greater than or equal to 130 mm Hg systolic or greater than or equal to 85 mm Hg diastolic, or treatment for or diagnosis of hypertension
- Fasting glucose 100 mg/dL or higher, or treatment for or diagnosis of hyperglycemia
Researchers used International Classification of Diseases (ICD-10 and ICD-9) medical billing codes to identify patients with primary open-angle glaucoma, regular or low-tension glaucoma, pigment dispersion glaucoma, and pseudoexfoliation glaucoma. Any of these conditions that resulted in GON were collectively analyzed and referred to as GON. Researchers identified patients with billing codes of OHTN in a similar fashion.
جدول. البيانات الديموغرافية الأساسية.
جدول. البيانات الديموغرافية الأساسية.
ارتباط متلازمة الأيض بالمياه الزرقاء وفرط ضغط دم العين
Baseline demographic data included age, sex, race or ethnicity, and smoking history. In patients with GON or OHTN, researchers reviewed the most recent eye exam and, if available for each eye, documented a logarithm of the minimum angle of resolution conversion for the best corrected or pinhole Snellen visual acuity, IOP, cup-to-disk ratio, and CCT.
CCT's role
Dr. Roddy summarizes the study outcomes: "After adjusting for baseline demographic data, we concluded that GON was not associated with MetS — and an increasing number of MetS components were also not associated with GON. Patients with GON and MetS, however, did have higher IOP and CCT than those patients without MetS.
"Both before and after adjustment for demographic factors, patients with MetS were more likely to have OHTN. Increasing numbers of MetS components were also associated with OHTN. After IOP was adjusted for CCT, there was no significant association between MetS and adjusted IOP in patients with GON and patients with OHTN. Our study supports prior evidence that MetS is associated with OHTN and also suggests that this association may be related to increased CCT."
For more information
Rochester Epidemiology Project.
Wu KY, et al. Association of metabolic syndrome with glaucoma and ocular hypertension in a Midwest United States population. Journal of Glaucoma. In press.
Refer a patient to Mayo Clinic.