Overview
Cardiac ablation
Cardiac ablation
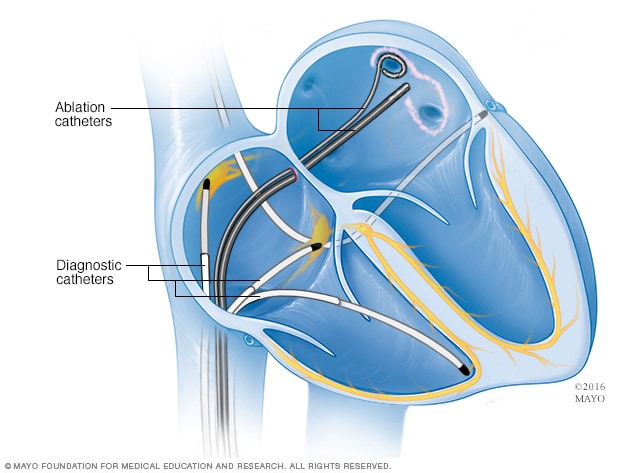
Cardiac ablation is a treatment for irregular heart rhythms, called arrhythmias. It uses thin, flexible tubes called catheters and heat or cold energy to create tiny scars in the heart. The scars block the faulty signals that cause irregular heartbeats. This illustration shows a type of cardiac ablation called pulmonary vein isolation.
Cardiac ablation is a treatment for irregular heartbeats, called arrhythmias. It uses heat or cold energy to create tiny scars in the heart. The scars block faulty heart signals and restore a typical heartbeat.
Cardiac ablation is most often done using thin, flexible tubes called catheters that are inserted through a blood vessel. Less commonly, ablation is done during heart surgery.
Products & Services
Types
Why it's done
Cardiac ablation is a treatment to stop or prevent irregular heartbeats, called arrhythmias.
An arrhythmia happens when the electrical signals that tell the heart to beat don't work as they should. The heart may beat too fast or too slow. Or the pattern of the heartbeat may be irregular.
Depending on the type of irregular heartbeat, cardiac ablation may be one of the first treatments. Other times, it's done when medicines or other treatments don't work.
A healthcare professional may recommend cardiac ablation if:
- Medicines to treat an irregular heartbeat don't work for you.
- Medicines to treat an irregular heartbeat cause you serious side effects.
- You have a type of irregular heartbeat that does well with this treatment, such as Wolff-Parkinson-White syndrome or supraventricular tachycardia.
- You have a high risk of sudden cardiac arrest or other complications.
Risks
The risks of cardiac ablation depend on the type of ablation and why it’s done. Possible risks may include:
- Bleeding or infection where the catheter was placed.
- Blood vessel damage.
- Heart valve damage.
- A new irregular heartbeat or one that gets worse.
- Slow heart rate, which may need a pacemaker to fix.
- Blood clots in the legs or lungs.
- Stroke or heart attack.
- Narrowing of the veins that carry blood between the lungs and heart, called pulmonary vein stenosis.
- Damage to the kidneys from contrast used during the procedure.
Discuss the risks and benefits with your healthcare team to understand if this treatment is right for you.
How you prepare
Before a cardiac ablation, you may have several tests to check your heart health.
You may need to stop eating and drinking the night before your procedure. Your care team tells you if you should continue or change any medicines before cardiac ablation.
What you can expect
Before
Cardiac ablation is done in the hospital. A member of your care team places an IV into your forearm or hand. You usually get medicines to help you relax. This is called sedation.
The amount of sedation needed for the treatment depends on the type of irregular heartbeat you have and your overall health. You may be fully awake or lightly sedated. Some people get a combination of medicines to put them in a sleep-like state. This is called general anesthesia.
During
Catheter insertion points for cardiac ablation
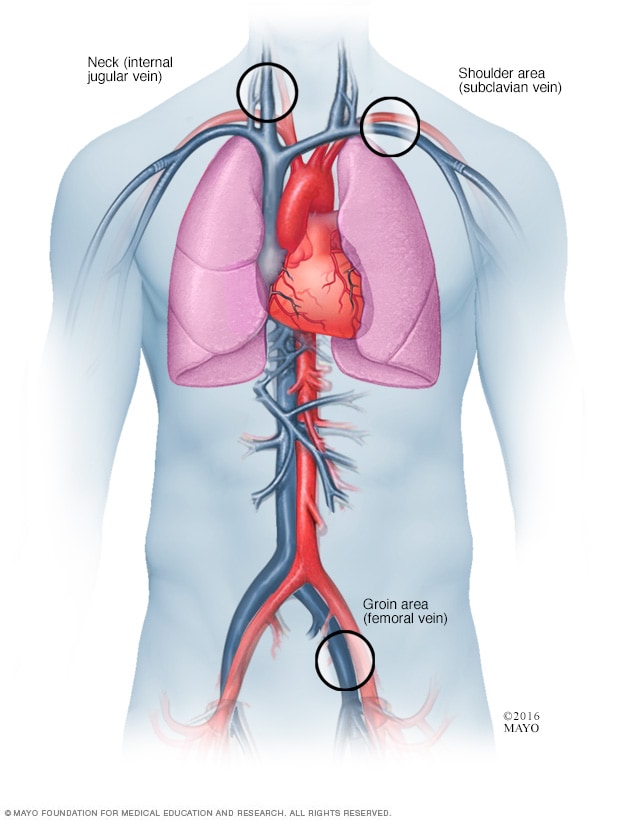
Catheter insertion points for cardiac ablation
During cardiac ablation, a thin, flexible tube called a catheter is passed through a blood vessel to reach the heart. More than one catheter is often used. The catheter may be inserted in the groin, the shoulder or the neck.
A doctor inserts one or more thin, flexible tubes called catheters into a blood vessel and guides them to the heart. These tubes are usually placed into a blood vessel in the groin. But sometimes, they are placed in the shoulder or neck.
Dye called contrast flows through the tube. The dye helps blood vessels show up more clearly on X-ray images.
Sensors on the tip of the catheter send electrical signals and record the heart's electrical activity. Your healthcare team uses this information to find the area that is causing the irregular heartbeats. The information also tells the doctor where to apply the treatment. This part of the procedure is called an electrophysiology (EP) study.
One of the following ablation methods is used to create small scars in the heart. The scars block the irregular heart rhythms:
- Heat, called radiofrequency energy.
- Extreme cold, called cryoablation.
You shouldn't feel any discomfort during the procedure. If you have bad pain or shortness of breath, tell your care team.
After
Cardiac ablation usually takes 3 to 6 hours to complete. The time depends on the type of irregular heartbeat being treated.
After the procedure, you rest in a recovery area for a few hours where a care team closely checks on you. Depending on your condition, you may go home the same day or spend the night in the hospital. Plan to have someone drive you home.
Some people feel a little sore after cardiac ablation. The soreness shouldn't last more than a week. Most people can return to their daily activities within a few days. Avoid heavy lifting for about a week.
Results
Most people see improvements in their quality of life after cardiac ablation. But there's a chance that the irregular heartbeat may return. If this happens, the treatment may be repeated or your healthcare professional might suggest other treatments. Depending on your type of irregular heartbeat, you may still need to take heart medicines after a cardiac ablation.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Feb. 02, 2024