Diagnosis
Tests to diagnose rectal cancer
Colonoscopy
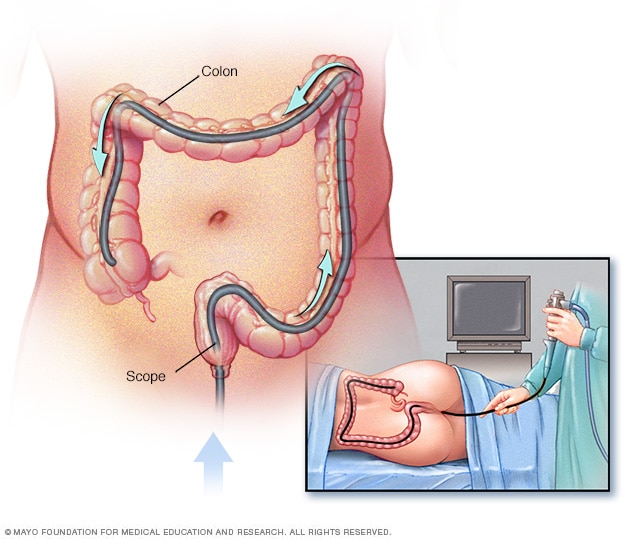
Colonoscopy
During a colonoscopy, the healthcare professional puts a colonoscope into the rectum to check the entire colon.
Rectal cancer can be found during a screening test for colorectal cancer. Or it may be suspected based on your symptoms. Tests and procedures used to confirm the diagnosis include:
- Using a scope to examine the inside of your colon and rectum (colonoscopy). Colonoscopy uses a long, flexible tube (colonoscope) attached to a video camera and monitor to view your colon and rectum. If cancer is found in your rectum, your doctor may recommend examining your colon in order to look for additional suspicious areas.
-
Removing a sample of tissue for testing (biopsy). If any suspicious areas are found, your doctor can pass surgical tools through the colonoscope to take tissue samples (biopsies) for analysis and remove polyps.
The tissue sample is sent to a lab to be examined by doctors who specialize in analyzing blood and body tissues (pathologists). Tests can determine whether the cells are cancer, whether they're aggressive and which genes in the cancer cells are abnormal. Your doctor uses this information to understand your prognosis and determine your treatment options.
Tests to look for rectal cancer spread
Once you're diagnosed with rectal cancer, the next step is to determine the cancer's extent (stage). The stage of your cancer helps determine your prognosis and your treatment options.
Staging tests include:
- Complete blood count (CBC). This test reports the numbers of different types of cells in your blood. A CBC shows whether your red blood cell count is low (anemia), which suggests that a tumor is causing blood loss. A high level of white blood cells is a sign of infection, which is a risk if a rectal tumor grows through the wall of the rectum.
- Blood tests to measure organ function. A chemistry panel is a blood test to measures levels of different chemicals in the blood. Abnormal levels of some of these chemicals may suggest that cancer has spread to the liver. High levels of other chemicals may indicate problems with other organs, such as the kidneys.
- Carcinoembryonic antigen (CEA). Cancers sometimes produce substances called tumor markers that can be detected in blood. One such marker, carcinoembryonic antigen (CEA), may be higher than usual in people with colorectal cancer. CEA testing is particularly useful in monitoring your response to treatment.
- CT scan of the chest. This imaging test helps determine whether rectal cancer has spread to other organs, such as the liver and lungs.
- MRI of the pelvis. An MRI provides a detailed image of the muscles, organs and other tissues surrounding a tumor in the rectum. An MRI also shows the lymph nodes near the rectum and different layers of tissue in the rectal wall.
Your doctor uses information from these tests to assign your cancer a stage. The stages of rectal cancer are indicated by Roman numerals that range from 0 to IV. The lowest stage indicates cancer that is limited to the lining of the inside of the rectum. By stage IV, the cancer is considered advanced and has spread (metastasized) to other areas of the body.
Treatment
Rectal cancer treatment often involves a combination of therapies. When possible, surgery is used to cut away the cancer cells. Other treatments, such as chemotherapy and radiation therapy, may be used after surgery to kill any cancer cells that remain and reduce the risk that cancer will return.
If surgeons are concerned that the cancer can't be removed completely without hurting nearby organs and structures, your doctor may recommend a combination of chemotherapy and radiation therapy as your initial treatment. These combined treatments may shrink the cancer and make it easier to remove during an operation.
Surgery
Rectal cancer is often treated with surgery to remove the cancer cells. Which operation is best for you depends on your particular situation, such as the location and stage of your cancer, how aggressive the cancer cells are, your overall health, and your preferences.
Operations used to treat rectal cancer include:
-
Removing very small cancers from the inside of the rectum. Very small rectal cancers may be removed using a colonoscope or another specialized type of scope inserted through the anus (transanal local excision). Surgical tools can be passed through the scope to cut away the cancer and some of the healthy tissue around it.
This procedure might be an option if your cancer is small and unlikely to spread to nearby lymph nodes. If a lab analysis finds that your cancer cells are aggressive or more likely to spread to the lymph nodes, your doctor may recommend additional surgery.
-
Removing all or part of the rectum. Larger rectal cancers that are far enough away from the anal canal might be removed in a procedure (low anterior resection) that removes all or part of the rectum. Nearby tissue and lymph nodes are also removed. This procedure preserves the anus so that waste can leave the body normally.
How the procedure is performed depends on the cancer's location. If cancer affects the upper portion of the rectum, that part of the rectum is removed and then the colon is attached to the remaining rectum (colorectal anastomosis). All of the rectum may be removed if the cancer is located in the lower portion of the rectum. Then the colon is shaped into a pouch and attached to the anus (coloanal anastomosis).
-
Removing the rectum and anus. For rectal cancers that are located near the anus, it might not be possible to remove the cancer completely without damaging the muscles that control bowel movements. In these situations, surgeons may recommend an operation called abdominoperineal resection (APR) to remove the rectum, anus and some of the colon, as well as nearby tissue and lymph nodes.
The surgeon creates an opening in the abdomen and attaches the remaining colon (colostomy). Waste leaves your body through the opening and collects in a bag that attaches to your abdomen.
Chemotherapy
Chemotherapy uses drugs to destroy cancer cells. For rectal cancer, chemotherapy might be recommended after surgery to kill any cancer cells that might remain.
Chemotherapy combined with radiation therapy might also be used before an operation to shrink a large cancer so that it's easier to remove with surgery.
Chemotherapy can also be used to relieve symptoms of rectal cancer that can't be removed with surgery or that has spread to other areas of the body.
Radiation therapy
Radiation therapy uses powerful energy sources, such as X-rays and protons, to kill cancer cells. In people with rectal cancer, radiation therapy is often combined with chemotherapy that makes the cancer cells more likely to be damaged by the radiation. It can be used after surgery to kill any cancer cells that might remain. Or it can be used before surgery to shrink a cancer and make it easier to remove.
When surgery isn't an option, radiation therapy might be used to relieve symptoms, such as pain.
Combined chemotherapy and radiation therapy
Combining chemotherapy and radiation therapy (chemoradiotherapy) makes cancer cells more vulnerable to radiation. The combination is often used for larger rectal cancers and those that have a higher risk of returning after surgery.
Chemoradiotherapy may be recommended:
- Before surgery. Chemoradiotherapy may help shrink the cancer enough to make a less invasive surgery possible. The combined treatment may increase the chance that your operation will leave the anal area intact so waste can leave the body normally after surgery.
- After surgery. If surgery was your first treatment, your doctor may recommend chemoradiotherapy afterward if there's an increased risk that your cancer may return.
- As the primary treatment. Your doctor may recommend chemoradiotherapy to control the growth of cancer if your rectal cancer is advanced or if surgery isn't an option.
Targeted drug therapy
Targeted drug treatments focus on specific abnormalities present within cancer cells. By blocking these abnormalities, targeted drug treatments can cause cancer cells to die.
Targeted drugs are usually combined with chemotherapy. Targeted drugs are typically reserved for people with advanced rectal cancer.
Immunotherapy
Immunotherapy is a drug treatment that uses your immune system to fight cancer. Your body's disease-fighting immune system may not attack your cancer because the cancer cells produce proteins that help them hide from the immune system cells. Immunotherapy works by interfering with that process.
Immunotherapy is usually reserved for advanced rectal cancer.
Supportive (palliative) care
Palliative care is focused on providing relief from pain and other symptoms of a severe illness. Palliative care specialists work with you, your family and your other doctors to provide an extra layer of support that complements your ongoing care.
Palliative care is provided by a team of doctors, nurses and other specially trained professionals. Palliative care teams aim to improve the quality of life for people with cancer and their families. This form of care is offered alongside curative or other treatments you may be receiving.
More Information
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Coping and support
A diagnosis of cancer can be overwhelming. With time you'll find ways to cope with the distress and uncertainty of cancer. Until then, you may find that it helps to:
- Learn enough about rectal cancer to make decisions about your care. Ask your doctor about your cancer, including your treatment options and, if you like, your prognosis. As you learn more about rectal cancer, you may become more confident in making treatment decisions.
- Keep friends and family close. Keeping your close relationships strong will help you deal with your rectal cancer. Friends and family can provide the practical support you'll need, such as helping take care of your home if you're in the hospital. And they can serve as emotional support when you feel overwhelmed by cancer.
-
Find someone to talk with. Find a good listener who is willing to listen to you talk about your hopes and fears. This may be a friend or family member. The concern and understanding of a counselor, medical social worker, clergy member or cancer support group also may be helpful.
Ask your doctor about support groups in your area. Or check with local and national cancer organizations, such as the National Cancer Institute or the American Cancer Society.
Preparing for your appointment
If your doctor suspects that you may have rectal cancer, you'll likely be referred to one or more specialists who treat rectal cancer, including:
- A doctor who treats digestive diseases (gastroenterologist)
- A doctor who treats cancer (oncologist)
- A surgeon specializing in procedures involving the colon and rectum (colorectal surgeon)
- A doctor who uses radiation to treat cancer (radiation oncologist)
Here are some things you can do before you meet with these doctors:
- Find out if there's anything you need to do before your appointment, such as avoid certain foods or medications.
- Make a list of all your medications, including vitamins or supplements.
- Consider taking a family member or friend along to take notes on what your doctors say, so that you can concentrate on listening.
- Write down questions to ask your doctor.
For rectal cancer, here are some questions you may want to ask:
- In what part of the rectum is my cancer located?
- What is the stage of my rectal cancer?
- Has my rectal cancer spread to other parts of my body?
- Will I need more tests?
- What are the treatment options?
- How much does each treatment increase my chances of a cure?
- What are the potential side effects of each treatment?
- How will each treatment affect my daily life?
- Is there one treatment that you feel is best for me?
- What would you recommend to a family member or friend in my same situation?
- How much time can I take to make my decision about treatment?
- Should I seek a second opinion?
- Are there any brochures or other printed material that I can take with me? What websites do you recommend?