Each type of psoriasis has different signs and symptoms and can look different on each person. It's possible to have more than one type at a time. Psoriasis occurs when the life cycle of skin cells speeds up, resulting in a rapid buildup of rough, dead skin cells. These skin cells build up and form dry, scaly patches.
Psoriasis patches can range from a few spots of dandruff-like scaling to major rashes that cover large areas. The condition is not passed from person to person.
Learn about the symptoms of common types of psoriasis.
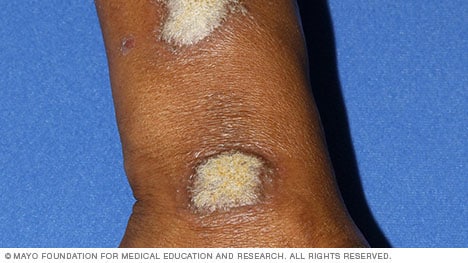 Plaque psoriasis
Plaque psoriasis
Plaque psoriasis, the most common form of psoriasis, causes dry, raised skin patches (plaques) covered with gray or silver scales. It may look different depending on your skin color, ranging from pink on white skin to brown or gray on brown or Black skin.
You may have just a few plaques or many. After the plaques clear up, the affected skin might temporarily be lighter (hypopigmentation) or darker (hyperpigmentation) than usual.
Your psoriasis may improve with certain lifestyle measures, such as:
- Taking daily baths
- Applying nonprescription cortisone cream and heavy, ointment-based moisturizer
- Learning to identify and avoiding personal triggers of psoriasis, such as stress
- Avoiding smoking
Moderate or severe cases may require light therapy, prescription steroid creams, coal tar products applied to the skin, oral or injected medications (systemic treatment), or a combination of these.
 Nail psoriasis
Nail psoriasis
Psoriasis can affect fingernails and toenails, causing pitting, abnormal nail growth and discoloration. Psoriatic nails may become loose and separate from the nail bed (onycholysis). Severe cases may cause the nail to crumble.
Nail psoriasis often accompanies another type of psoriasis, such as plaque psoriasis. Treatment options include oral or injected medications.
 Guttate psoriasis
Guttate psoriasis
Guttate psoriasis is more common in children and young adults. It's usually triggered by a bacterial infection such as strep throat. Guttate psoriasis appears as small, water-drop-shaped spots on the trunk, arms or legs. These spots are typically covered by a fine scale.
Guttate psoriasis typically responds to treatment, which includes light therapy, prescription steroid creams and oral medications. It may also improve with treatment of the underlying cause or infection, if identified.
 Inverse psoriasis
Inverse psoriasis
Inverse psoriasis causes smooth patches of inflamed skin, usually under the breasts and around the groin and buttocks.
Treatment options include nonprescription corticosteroid ointments or other prescription-strength creams or ointments.
 Pustular psoriasis
Pustular psoriasis
Pustular psoriasis causes clearly defined pus-filled sores. It can occur in widespread patches or in smaller areas on the palms or soles, as shown here. This rare form of psoriasis can develop quickly, with blisters forming just hours after your skin becomes inflamed and sore. The blisters clear up within several days, but recur. Possible causes include medication withdrawal and infection.
Small patches of pustular psoriasis may be treated with a corticosteroid ointment. Larger patches usually require prescription oral medication, elimination of the underlying cause, if possible, and other topical and oral or injected (systemic) therapies. Light therapy may be useful once the blisters clear up and the skin is less irritated.
 Erythrodermic psoriasis
Erythrodermic psoriasis
Erythrodermic psoriasis is the least common type of psoriasis. It can cover the entire body with a scaly rash that can itch or burn intensely. It may be triggered by corticosteroids or other medications, severe sunburn, or another type of psoriasis.
Treatment of erythrodermic psoriasis usually requires prescription oral medication, medicated wet dressings and topical steroids. For severe disease, you might need a combination of therapies and hospital care.
Dec. 14, 2023
- AskMayoExpert. Psoriasis. Mayo Clinic; 2021.
- Dinulos JGH. Psoriasis and other papulosquamous diseases. In: Habif's Clinical Dermatology. 7th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed March 5, 2020.
- Kelly AP, et al., eds. Psoriasis. In: Taylor and Kelly's Dermatology for Skin of Color. 2nd ed. McGraw Hill; 2016. https://accessmedicine.mhmedical.com. Accessed Sept. 13, 2021.
- Bolognia JL, et al., eds. Psoriasis. In: Dermatology. 4th ed. Elsevier; 2018. https://www.clinicalkey.com. Accessed March 5, 2020.
- Feldman SR, et al. Psoriasis: Epidemiology, clinical manifestations, and diagnosis. https://www.uptodate.com/contents/search/. Accessed Sept. 15, 2021.