Overview
Stereotactic body radiotherapy (SBRT) is a type of noninvasive treatment that uses precisely focused radiation beams to treat tumors. The beams come from different angles and give a high dose of radiation to the tumor while helping protect nearby healthy tissue.
SBRT can be used in many parts of the body, including the lung, liver, bone, lymph nodes, prostate, breast, kidneys, head and neck, and other soft tissues. It can be used for both cancerous and noncancerous targets.
Traditional radiation therapy is given in small doses over many sessions. SBRT is different. It delivers a higher dose in only 1 to 5 treatments using very precise targeting. The number of treatments depends on the target and location within the body.
SBRT is sometimes called stereotactic ablative radiotherapy (SABR). Ablative means the radiation dose is high enough to destroy the tumor cells or noncancerous target in the treated area. When used on the brain, SBRT is called stereotactic radiosurgery (SRS).
Types of stereotactic body radiotherapy (SBRT)
Types of SBRT include:
- Linear accelerator (LINAC). A LINAC machine uses X-rays, also known as photons. This is the most common type of SBRT used today.
- Proton beam, also called charged particle. This type uses protons instead of X-rays. Proton therapy may be used for targets that are close to important organs or in areas that have had radiation before.
Other types of radiation therapy
Other types of radiation treatments include intensity-modulated radiation therapy (IMRT) and external beam radiation therapy (EBRT). Unlike SBRT, these types of radiation therapies are given in smaller doses over many sessions. These longer treatments are used when a slower, gradual approach is safer for nearby healthy tissue.
Products & Services
Why it's done
Stereotactic body radiotherapy (SBRT) is used to treat small, well-defined targets with high precision. It may be recommended when surgery is not possible or not the safest option, or in select cases when only a limited number of areas need treatment.
SBRT may be considered when:
- It offers better outcomes than traditional radiation for some cancers.
- Surgery cannot be performed safely.
- Targets are close to important organs or are hard to reach and need very precise treatment.
- A target is in an area that was treated with radiation before and a second course cannot be given safely with conventional treatment.
- Cancer has only spread to a limited number of areas in the body, sometimes called oligometastatic disease. Treating these areas can help control the disease and relieve symptoms.
SBRT also may delay the need to start or change treatments such as chemotherapy or hormone therapy.
Risks
Side effects from stereotactic body radiotherapy (SBRT) often depend on the part of the body being treated. Many people have mild symptoms that last for a short time.
Early side effects
Early side effects usually occur during treatment or shortly afterward and are often short-term. They can include:
- Fatigue. Extreme tiredness can occur for the first few days after SBRT.
- Swelling. Swelling at or near the treatment site can cause symptoms such as a short-term increase in pain. A healthcare professional might prescribe medicines to prevent or treat these symptoms.
- Nausea or vomiting. Treatment for a tumor near the bowel or liver might cause these symptoms for a short time.
- Skin changes. Skin in the treatment area can become irritated, itchy or dry.
Late side effects
Rarely, side effects can appear months or years after treatment. These might include:
- Weakened bones that can break.
- Changes in bowel or bladder habits.
- Changes in the lungs or breathing.
- Changes in the spinal cord or nearby nerves.
- Swelling in the arms or legs, also known as lymphedema.
- Very rarely, development of a new cancer.
Not everyone experiences side effects, and risks vary based on the treatment area and individual health factors.
How you prepare
Preparation for stereotactic body radiotherapy varies depending on the condition and body area being treated.
Food and medications
There are usually no restrictions or changes in your diet. In some cases, such as abdominal treatments, you may fast for up to four hours before treatment. Some people may take medicine to help with pain, nausea or anxiety.
Medical devices
Tell your healthcare team if you have medical devices inside your body. These might include a pacemaker, artificial heart valve, aneurysm clips, neurostimulators or stents.
What you can expect
SBRT is usually an outpatient procedure. This means you likely won't need to stay in the hospital after treatment.
Each treatment takes 30 to 60 minutes. Ask a member of your healthcare team if you'll need to have someone with you.
SBRT is not painful. You lie still on a treatment table while the machine moves around you to deliver radiation. You can talk to your care team during treatment. Your care team monitors you closely.
All SBRT delivers focused high-dose radiation to the treatment target while limiting the radiation to nearby healthy tissue. The high dose of radiation allows treatment to be delivered in fewer treatments than traditional radiation.
The radiation works over a period of time to control the treated target. The full effects of SBRT may continue to develop over weeks to months after treatment is completed.
Most people can return to their usual activities within a day or two, depending on how they feel.
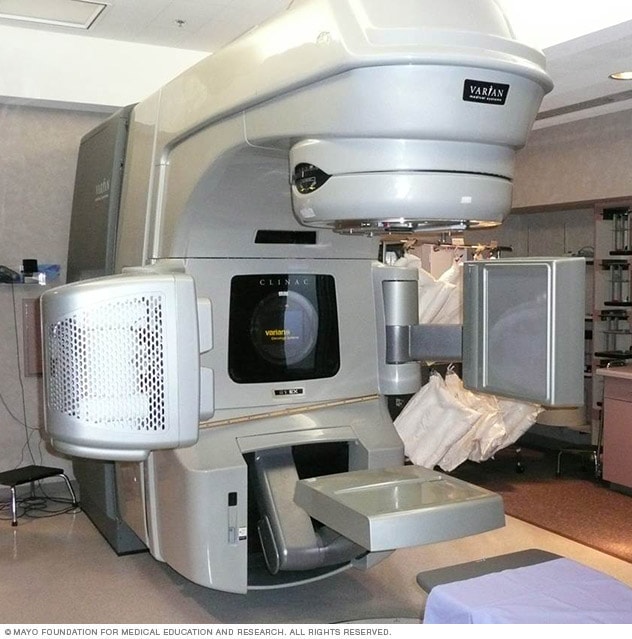 LINAC machine
LINAC machine
Stereotactic body radiotherapy machines use many precisely focused radiation beams to treat tumors and other problems all over the body.
Before the procedure
Your healthcare team takes several steps before stereotactic body radiotherapy (SBRT). Steps might include:
- Body positioning. To target your treatment exactly, you need to remain in one position and stay completely still. Your healthcare team finds the best position for your body. Often this involves using custom devices to hold you in place and keep you comfortable.
- Target positioning. Markers help target treatment. Often, tattoos on the skin keep the area marked for repeated treatments. Sometimes it's necessary to place a small metal marker, known as a fiducial marker, in or near the tumor. The fiducial marker is about the size of a grain of rice.
- Imaging. Once you're in place, imaging scans get information about your tumor, including location, size and shape. A scan also can show how the tumor moves while you breathe. Sometimes, the information gathered might show that you might need to hold your breath for 10 to 30 seconds at a time during treatment to keep the tumor still.
- Planning. Your healthcare team uses the imaging scans and specialized software to plan the best approach to treatment to meet your needs.
During the procedure
If you feel anxious, talk with your care team before treatment. Team members can explain what to expect and help you feel more comfortable. You may be offered medicine to help you relax.
 LINAC stereotactic radiosurgery preparation
LINAC stereotactic radiosurgery preparation
To prepare for stereotactic body radiotherapy, devices are used to help the person undergoing treatment to hold still. The type of devices used will depend on which part of the body is being treated. Here, a customized cushion provides support and a plastic sheet holds the person in place.
After the procedure
After the procedure, you can expect the following:
- If you have symptoms such as a temporary increase in pain or nausea, ask for medicines to treat them.
- You'll be able to eat and drink after the procedure.
- Usually, you can go home the same day.
- You can usually get back to regular activities within a day or two.
Results
The effects of SBRT happen over a period of time. What happens after treatment depends on the condition being treated and the location of the target. SBRT might result in the following:
- For noncancerous targets, the goal is often to stop growth or reduce activity of the target. The target may shrink slowly with time. Or it may stay the same size and that may still be considered a good response.
- For cancerous targets, the treated tumor may shrink with time, or it may stop growing. Changes are not always seen right away. Early imaging can sometimes show temporary swelling or inflammation related to treatment.
You may have follow-up exams and tests to monitor your progress after stereotactic body radiotherapy.
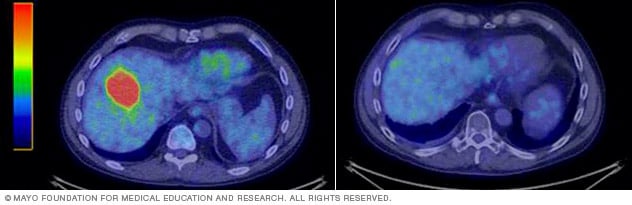 Liver tumor before and after SBRT
Liver tumor before and after SBRT
Tumor in the liver before (left) and after (right) stereotactic body radiotherapy.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Feb. 06, 2026