Jan. 06, 2018
Editor's note
Over the course of 2018, this newsletter will feature key aspects of the performance improvement (PI) process, including event identification, levels of review, action planning and event resolution.
Performance improvement
With a culture of safety laying the groundwork, performance improvement (PI) can flourish. PI is a linear process, following an orderly sequence of steps from event identification through event resolution and loop closure.
Though patient harm may come to mind when considering PI, harm is not a mandatory component that prompts a review. Rather, PI is about a mindset of assessing what could have been done better, irrespective of outcome. If harm has occurred, the objective is to ensure whatever situation or event has arisen does not recur and that the issue is addressed.
"PI is not solely motivated by patient harm," says Brian D. Kim, M.D., a trauma surgeon and adult trauma medical director at Mayo Clinic in Rochester, Minnesota. "Even though a trauma patient may have an excellent outcome, we can still dissect the patient's care and find opportunities for improvement, not only for that patient's care but for the next patient."
PI is quintessential not only to trauma care but also to medical care delivery in general. Trauma has emerged as a leader in this arena, as the time sensitivity, acuity and multidisciplinary teams within trauma lend themselves to looking at how all parties come together to care for a particular patient as well as the spectrum of patients treated. Dr. Kim describes a PI mentality as recognizing that trauma care is bigger than just one patient: It is ensuring care for all is as robust as it can be.
"The mindset is the No. 1 thing in performance improvement — it's having members of the team who care for trauma patients understand that good is good, better is better than good — but having the mindset that we can always improve on better," says Dr. Kim. "We can always seek to improve and optimize the care, and not be satisfied with just the end result. It's the process that helps the patient and the next patient thereafter."
Robust PI is a large endeavor, and challenging to work through, yet critical to continuous improvement in trauma care.
About event identification
Trauma PI filter tracking worksheet
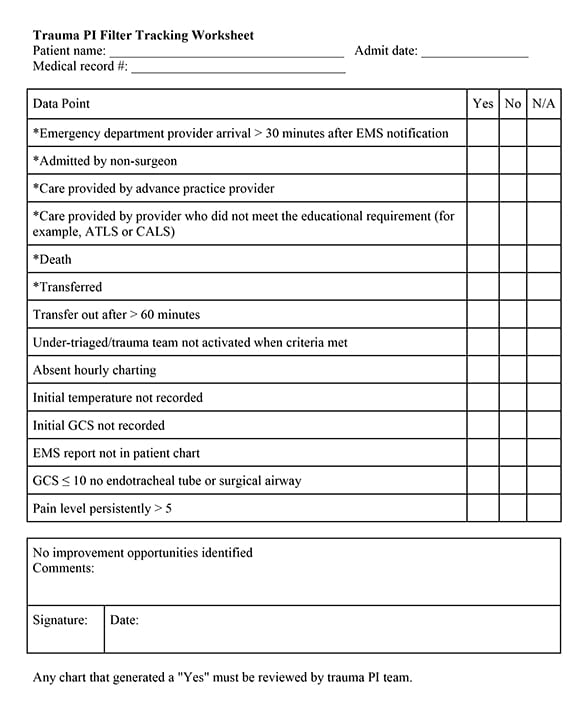
Trauma PI filter tracking worksheet
Sample of a trauma PI filter tracking worksheet, reprinted with permission from the Minnesota Department of Health.
The first measuring stick for successful care for all trauma patients is an examination of an individual trauma patient's care. Thus, event identification — pointing out an issue in one patient's experience — is the first step in the PI process.
Events can be identified through a number of sources, but the following are the principal means:
Individual or group report
Anyone who ever touches — figuratively as well as literally — a trauma patient should have a voice in identifying events for review. Issue identification can come from parties as diverse as prehospital personnel, health system affiliates, administration, trauma performance improvement coordinators, trauma medical directors, subspecialty surgeons, or personnel from nursing, radiology, rehabilitation, ICU or admission transfer services. In addition to medical personnel, trauma patients themselves also may identify events.
Any of these trauma care participants should consider identifying an event according to the "CUS words" principle:
- Concern. If a patient or provider has a concern about something involved in the care, a reportable event may have occurred. An example of this type of concern would be a nurse feeling uneasy about how resuscitation was delivered to a patient.
- Uncomfortable. When trauma providers or their patients feel uncomfortable with any aspect of the care, they should look at whether an event transpired that merits review. For instance, an imaging technician might feel uncomfortable with a lengthy transfer delay for a patient critically injured in a car crash due to an emergency department physician insisting on imaging being completed first.
- Safety. If anyone involved in a trauma patient's care, inclusive of the patient, is uncertain whether the patient is safe at any time, this also may be a reason to report an event. For example, a physician may observe a nurse putting a trauma patient at risk of falling.
Audit filters
Designated criteria prompting a forced review (audit filters) also play an important role in identifying events. Examples of minimum mandatory events that must be reviewed are outlined for the state's trauma centers. Most often, such events come to light when data abstractors or trauma coordinators enter patient care data into the trauma registry, forwarding on any events meeting audit filter criteria to trauma leadership.
One example of an audit filter would be a double transfer from a Level IV to a Level II trauma center, then to a Level I center. The question to be reviewed in this case would be: Did that patient actually meet the criteria to go directly to the Level I trauma center? This question would prompt an examination of the transfer criteria at the Level IV hospital to see what might have led to two transfers, causing delay.
Another audit filter is a patient who dies while in trauma care, which automatically prompts the highest tier review.
"As medical director of Mayo Clinic Trauma Center, I know about all patients who succumb to their injuries," says Dr. Kim. "If there is an identified issue or opportunity for improvement that led to a patient's mortality, that's a weighty issue that needs to be closely examined."
Perspectives on event identification
In event identification, the objective is to gain clarity about a situation. Other steps in the PI process will then ensue, putting the event through a review sequence that will ultimately result in action, such as making system changes or supplying education for providers. If any harm has taken place, the goal would be to mitigate any further damage and take steps to ensure whatever situation or event transpired is appropriately addressed.
Dr. Kim suggests seven key takeaways for setting the stage for optimal event identification:
- All levels of trauma providers have a responsibility for and a role in PI.
- The culture of PI needs to be open and transparent.
- Making PI nonpunitive is critical.
- The motivation for PI should be optimizing the care for the injured patient.
- Though common principles apply (see CUS principles), event identification is not always standardized. The process of performance improvement needs to be customized to the medical center and providers involved.
- The individual or group bringing issues forward needs to be protected.
- Feedback to the person reporting an event or issue is appreciated and often provides positive reinforcement that the input was valuable.
"The more eyes, hands and heads involved in PI, the better," says Dr. Kim. "If there's an issue, we're all ears."