Jan. 18, 2019
3D-printed model of a pediatric patient's airway
3D-printed model of a pediatric patient's airway
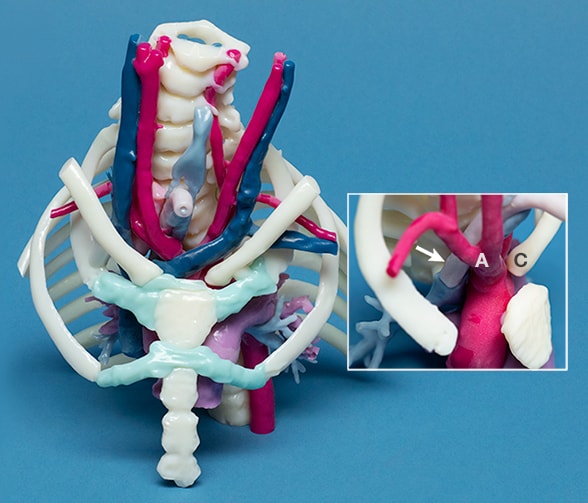
Photograph shows a 3D-printed model of a pediatric patient's airway, including airway-vascular relationships. The model clearly shows the innominate artery (A) and the displaced clavicle (C) driving the tracheostomy tube back to erode through the posterior tracheal wall (arrow). Mayo Clinic creates these models to aid in planning surgeries and explaining procedures to family members. The actual-size models follow patients from the operating rooms to their hospital rooms to help ensure smooth postoperative care.
Mayo Clinic Children's Center is one of the few centers in the United States where pediatric interventional pulmonology is part of daily practice. Mayo's pediatric pulmonologists can provide expert diagnostic and interventional bronchoscopy spanning infancy into adulthood for patients with breathing problems ranging from common to extremely challenging. Collaboration with other Children's Center specialists typically results in a treatment plan within days, even for children with complex conditions.
"In most centers, interventional bronchoscopy procedures are performed by adult specialists. However, as pediatric pulmonologists, we have enhanced understanding of the relevant indications for bronchoscopy in the pediatric population, and as part of a pediatric care team, we have a natural working relationship with other specialists," says R. Paul Boesch, D.O., chair of Pediatric Pulmonology at Mayo Clinic Children's Center in Rochester, Minnesota. "A solid, trusting relationship between the pulmonologist and anesthesiologist is essential for the safety and effectiveness of these procedures."
Mayo Clinic Children's Center performs between 400 and 500 pediatric bronchoscopies a year, for conditions including:
- Persistent wheezing that doesn't respond to asthma medications
- Chronic cough and recurrent infections
- Aerodigestive problems
- Anatomic anomalies that might require surgery
- Severe scoliosis that affects breathing
Indications for bronchoscopy
For children with chronic or recurrent breathing problems, bronchoscopy commonly yields information resulting in treatment changes, both medical and surgical. Dr. Boesch notes that bronchoscopy is an appropriate evaluation for children with:
- Noisy breathing
- Poorly controlled asthma, or persistent wheezing or cough
- Recurrent chest infections
- Feeding and swallowing difficulties
- Airway masses
- Obstructive sleep apnea
"We find that a very high percentage of children with persistent or atypical wheezing or poorly controlled asthma have either infectious problems that can be treated or anatomic problems that exacerbate the wheezing," Dr. Boesch says. "Sometimes anatomic problems can be addressed with surgery. If not, we might be able to scale back some of the asthma therapies that may not be having an effect — which is beneficial in terms of avoiding cost and side effects."
Patients with complex airway problems often have both flexible and rigid bronchoscopy, performed in a single procedure by a pediatric pulmonologist and a pediatric otolaryngologist, respectively. "The two techniques are highly complementary and together provide the most complete evaluation of the airway. Both providers see the airway together but bring different perspectives. This provides a seamless team approach to airway reconstruction," Dr. Boesch says.
Any additional testing, such as gastrointestinal endoscopy, can be done in the same procedure, avoiding multiple rounds of anesthesia, radiation exposure and clinic visits. "We prepare an itinerary for patients in which all tests and evaluations are completed within days. Our specialists then agree on a unified care plan," Dr. Boesch says.
For children with early-onset, congenital or neuromuscular scoliosis, pediatric pulmonologists consult early with orthopedic surgeons to identify airway and respiratory risks and to help guide the surgical approach. The pediatric pulmonologist can help manage the airway during surgery and prevent breathing complications after surgery. Similar support is often provided to cardiothoracic surgeons when vascular anomalies are compressing a patient's airway.
"Integrating pediatric pulmonologists into surgical teams is very beneficial and common here at Mayo," Dr. Boesch says. "We can often identify new findings and perform novel interventions based on our wide experience with interventional bronchoscopy and a team approach to care."