Descripción general
Resonancia magnética intraoperatoria
Resonancia magnética intraoperatoria
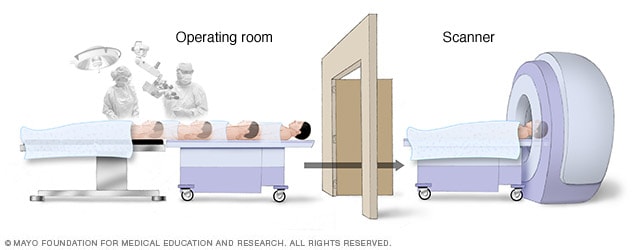
Debido a que el cerebro puede desplazarse durante la cirugía, las técnicas de cartografía cerebral y las imágenes por resonancia magnética intraoperatoria crean imágenes precisas del cerebro que guían al neurocirujano para extirpar de manera eficaz solo el tumor y evitar cualquier otro tejido cerebral a fin de preservar las funciones motrices, del lenguaje y otras funciones cerebrales importantes.
En la cirugía de cerebro asistida por computadora, los cirujanos utilizan tecnologías de obtención de imágenes para crear un modelo en 3D del cerebro.
La obtención de imágenes puede incluir resonancia magnética, resonancia magnética intraoperativa, tomografía computarizada y escaneos mediante tomografías por emisión de positrones.
El software de fusión especializado permite utilizar múltiples tipos de obtención de imágenes.
La obtención de imágenes puede hacerse antes de la cirugía y a veces se hace durante la cirugía.
Este modelo le permite al cirujano del cerebro, que se conoce como neurocirujano, planificar la manera más segura de tratar tu afección que requiere de cirugía.
Durante la cirugía, el sistema por computadora guía con precisión al cirujano hacia las áreas del cerebro que requieren tratamiento.
Por qué se realiza
Estimulación cerebral profunda
Estimulación cerebral profunda
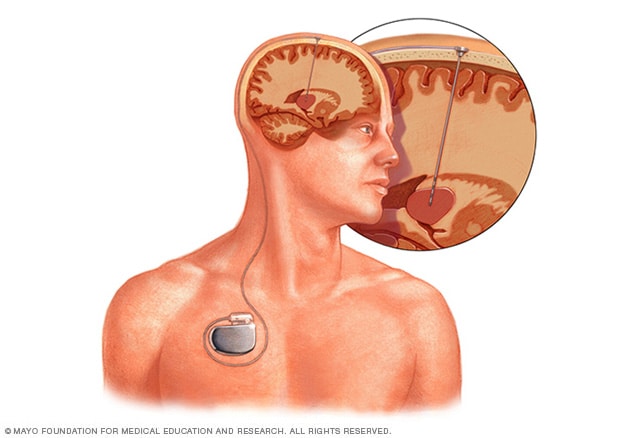
La estimulación cerebral profunda consiste en colocar un electrodo dentro del cerebro. La estimulación generada por el electrodo se controla mediante un dispositivo que se coloca debajo de la piel del pecho. Un cable que va por debajo de la piel conecta el dispositivo con el electrodo.
La cirugía de cerebro asistida por computadora se utiliza para tratar varias afecciones que afectan el cerebro.
Las afecciones incluyen tumores cerebrales, enfermedad de Parkinson, epilepsia y malformaciones arteriovenosas.
Si tienes un tumor cerebral, el cirujano puede combinar la cirugía asistida por computadora con la cirugía de cerebro con el paciente despierto.
Los neurocirujanos también utilizan técnicas asistidas por computadora cuando usan haces de radiación enfocados con precisión, que se conoce como radiocirugía estereotáctica.
La radiocirugía estereotáctica se puede usar para tratar tumores cerebrales, malformaciones arteriovenosas, neuralgia del trigémino y otras afecciones.
La cirugía asistida por computadora puede usarse durante el implante de electrodos para estimulación cerebral profunda o neuroestimulador sensible.
Los cirujanos pueden usar imágenes por resonancia magnética o tomografías computarizadas para mapear el cerebro y trazar la ubicación de los electrodos.
Esto se puede hacer si tienes temblor esencial, enfermedad de Parkinson, epilepsia, distonía o trastorno obsesivo compulsivo.
Riesgos
La cirugía cerebral asistida por computadora ayuda a reducir los riesgos de las cirugías.
Al crear un modelo tridimensional de tu cerebro, el neurocirujano puede planificar la forma más segura de tratar tu afección.
La asistencia informática también ayuda a guiar al cirujano hasta las zonas precisas del cerebro que necesitan tratamiento.
Sin embargo, toda cirugía conlleva algún riesgo.
La radiocirugía estereotáctica tiene pocos riesgos y los posibles efectos secundarios suelen ser temporales.
Pueden incluir sensación de mucho cansancio, dolor e hinchazón en el lugar del tratamiento.
Los efectos secundarios también pueden incluir irritación del cuero cabelludo.
En raras ocasiones, pueden producirse cambios cerebrales meses después de la intervención.
La estimulación cerebral profunda también conlleva riesgos como infección, hemorragias, convulsiones y accidentes cerebrovasculares.
Si se extirpa parte del cráneo para la cirugía, los riesgos potenciales incluyen hemorragias, inflamación o infección.
Cómo prepararte
Sigue las instrucciones de tu equipo de atención médica sobre lo que debes hacer en los días y horas previos a la cirugía cerebral.
Es posible que tengas que dejar de tomar ciertos medicamentos antes de la cirugía.
Por ejemplo, los medicamentos anticoagulantes retardan el proceso de coagulación.
Estos medicamentos pueden aumentar el riesgo de sangrado.
Habla con tu equipo de atención médica sobre si debes dejar de tomar anticoagulantes antes de la cirugía y durante cuánto tiempo.
Qué esperar
Lo que ocurra durante la cirugía cerebral asistida por computadora dependerá del tipo de cirugía a la que te sometas.
En la cirugía cerebral asistida por computadora se suele usar un medicamento que te sume en un estado similar al sueño, conocido como anestesia general.
Si te sometes a una cirugía cerebral con paciente despierto, se te administran medicamentos para relajarte y bloquear el dolor, pero estarás despierto.
Esto te permite interactuar con el equipo quirúrgico para maximizar la seguridad durante la intervención.
A veces, se extrae un trozo del cráneo para operar el cerebro.
En otras cirugías, como la radiocirugía estereotáctica, no se hacen cortes.
En cambio, la radiación se dirige a la zona del cerebro que necesita tratamiento.
Tu neurocirujano puede tomar imágenes durante la cirugía, conocidas como imágenes por resonancia magnética o tomografías computarizadas intraoperatorias, usando un escáner portátil de tomografía computarizada.
La máquina que se usa para tomar las imágenes puede estar en el quirófano en que te encuentras.
O puede estar en una sala contigua, en cuyo caso, serás trasladado hasta allí para obtener las imágenes.
Resultados
La cirugía cerebral asistida por computadora ayuda a los cirujanos a planificar y realizar las cirugías cerebrales con mayor precisión.
Cuando la cirugía cerebral es más precisa, se obtienen mejores resultados y menos complicaciones.
El uso de imágenes durante la cirugía, conocidas como imágenes por resonancia magnética o tomografías computarizadas intraoperatorias, ayuda a los neurocirujanos a tener en cuenta los cambios que se producen en el cerebro durante la cirugía.
Por ejemplo, el cerebro puede cambiar durante la intervención.
La toma de imágenes durante la cirugía ayuda a que esta sea más precisa.
Las imágenes intraoperatorias también alertan a los cirujanos de las complicaciones para que puedan resolverlas rápidamente.
Algunas investigaciones demostraron que el uso de resonancias magnéticas intraoperatorias ayuda a los cirujanos a extirpar más completamente un tumor o tejido dañado.
La cirugía cerebral asistida por computadora también permite preservar más tejido sano y centrarse únicamente en el tejido cerebral que se va a operar.