Jan. 15, 2021
A 58-year-old woman presented to the Endocrine Clinics at Mayo Clinic in Rochester, Minnesota, with symptoms of chest pressure, palpitations, insomnia and an unintentional weight loss of 20 kg over five months. She had a smoking history of 20 pack-years. There was no known family history of thyroid dysfunction, autoimmune disease or malignancy.
Physical examination revealed a diffusely enlarged thyroid gland (estimated weight of 50 grams), irregularly irregular heartbeats with a resting rate of 150 beats per minute, fine tremors of her fingers and brisk deep tendon reflexes.
Pruebas de laboratorio
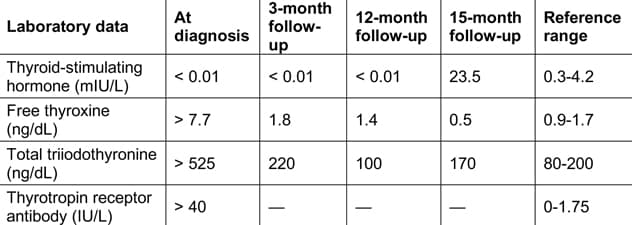
Pruebas de laboratorio
El hipertiroidismo grave y los altos niveles del anticuerpo receptor de tirotropina requieren significativas pruebas de laboratorio.
An electrocardiogram showed atrial fibrillation. The patient's laboratory work-up was significant for severe hyperthyroidism and elevated thyrotropin receptor antibody.
TAC del pecho en la presentación inicial
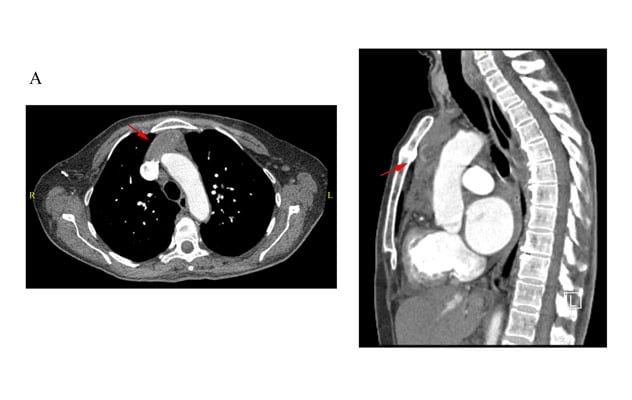
TAC del pecho en la presentación inicial
La tomografía computarizada (TAC) del pecho muestra un tumor mediastinal anterior homogéneo (flechas rojas) en la presentación inicial.
Chest computerized tomography (CT) angiogram to rule out pulmonary embolism was obtained prior to the thyroid function test results, which incidentally revealed an anterior mediastinal mass. The iodine 123 uptake scan demonstrated a symmetrically enlarged thyroid with diffuse homogeneous uptake (71% at 24 hours, reference range: 8% to 29%), without ectopic uptake in the chest.
Graves' disease was diagnosed and the patient was started on methimazole, 20 mg three times daily, and propranolol immediately. She was treated with radioactive iodine ablation (iodine 131, 20 millicuries) at seven-month follow-up. Her symptoms and thyroid function gradually improved. The patient eventually developed hypothyroidism and required thyroid hormone replacement at 15-month follow-up.
TAC del pecho en la cita de seguimiento de los tres meses
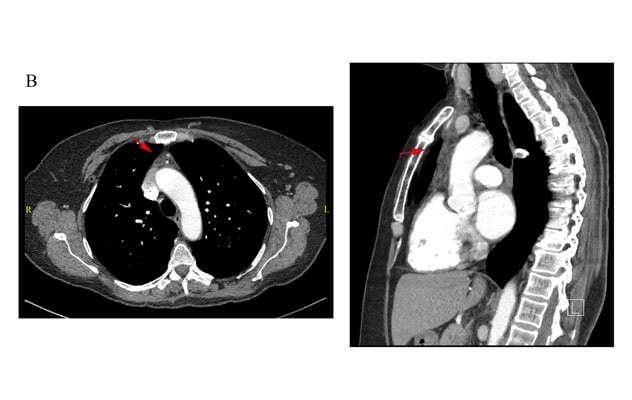
TAC del pecho en la cita de seguimiento de los tres meses
La tomografía computarizada (TAC) del pecho muestra un tumor mediastinal anterior homogéneo (flechas rojas) en la cita de seguimiento de los tres meses.
TAC del pecho en la cita de seguimiento de los 12 meses
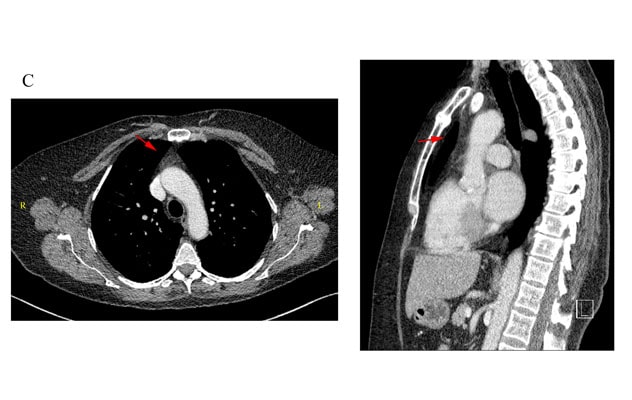
TAC del pecho en la cita de seguimiento de los 12 meses
La tomografía computarizada (TAC) del pecho muestra un tumor mediastinal anterior homogéneo (flechas rojas) en la cita de seguimiento de los 12 meses.
Repeat chest CT at three months and 12 months demonstrated significant decrease of the thymic volume.
Discussion
First described by Dr. William Halsted in Transactions of the American Surgical Association in 1914, thymic hyperplasia in Graves' disease is not uncommon, although the true incidence is unclear because chest imaging is not routinely obtained in every patient who is newly diagnosed with Graves' disease. The pathogenesis is thought to be related to a direct trophic effect from excess thyroid hormones, as well as autoimmunity from thyrotropin receptor antibody, leading to increased proliferation of cortical epithelial cells and medullary lymphoid follicles.
Diagnóstico diferencial de tumor mediastinal anterior
Diagnóstico diferencial de tumor mediastinal anterior
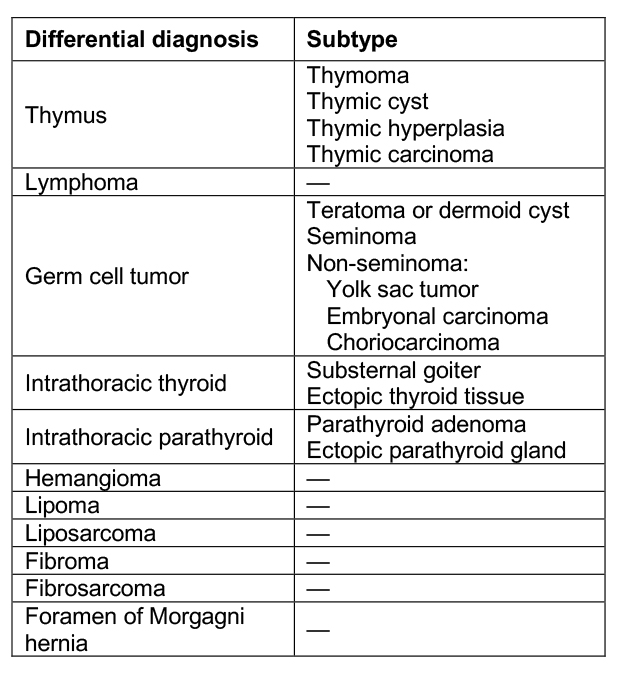
Al pensar en la etiología de un tumor mediastinal anterior, la lista de diagnósticos diferenciales es amplia.
When considering the etiology of an anterior mediastinal mass, the list of differential diagnoses is extensive. Overall, in cases unrelated to thyroid disease, the risk of malignancy of an anterior mediastinal mass is reportedly as high as 59% in patients ages 20 to 40, and 30% in other age groups. Therefore, obtaining a tissue biopsy or diagnostic thymectomy is often warranted.
However, in the setting of untreated thyrotoxicosis, this intervention should be strictly avoided as it is associated with critical complications such as triggering thyroid storm and leading to morbidity and mortality. Therefore, it is recommended that, in the absence of suspicious radiographic features (that is, heterogeneous enhancement, invasion of surrounding structures, calcification), medical treatment of Graves' disease with the goal of euthyroidism should be the next step and biopsy or thymectomy should be deferred in the acute setting.
Thymic hyperplasia in Graves' disease is a benign condition and often reversible to various degrees with treatment. Various studies have reported a significant decrease (33% to 90%) in thymic volume after successful treatment of hyperthyroidism using anti-thyroid drugs with a follow-up ranging from six weeks to two years. Therefore, a repeat chest image six months after achieving euthyroidism is recommended. If there is less than 50% regression of the mass, biopsy or thymectomy should be reconsidered to rule out malignancy.
Key points
- Thymic hyperplasia in Graves' disease is related to excess thyroid hormones and thyrotropin receptor antibody.
- It is a benign condition and usually improves after successful treatment of Graves' disease.
- Biopsy and thymectomy should be deferred in the setting of thyrotoxicosis and be reconsidered if thymus fails to regress on repeat imaging.