Descripción general
Aneurisma cerebral
Aneurisma cerebral
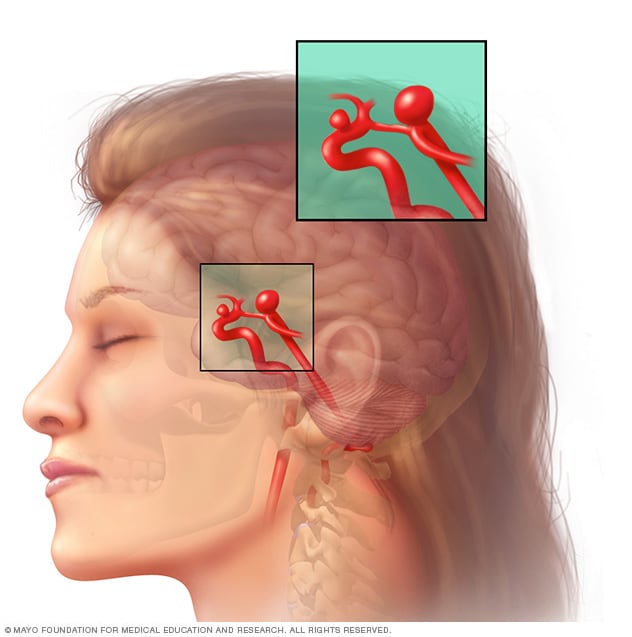
Un aneurisma es un abombamiento en un punto débil de las paredes de una arteria. Las paredes de un aneurisma pueden ser lo suficientemente finas como para que se rompan. La ilustración muestra a una persona con un aneurisma intacto. En el recuadro se muestra lo que sucede cuando un aneurisma se rompe.
Un aneurisma cerebral, también llamado aneurisma intracraneal, es una protuberancia o abombamiento en un vaso sanguíneo del cerebro. En ocasiones, un aneurisma tiene el aspecto de una cereza que cuelga de un tallo.
Los expertos creen que los aneurismas cerebrales se forman y crecen porque la sangre que fluye por el vaso sanguíneo ejerce presión sobre una zona débil de la pared del vaso. Esto puede causar un aumento del tamaño del aneurisma cerebral. Si el aneurisma cerebral presenta un derrame o se rompe, puede causar sangrado en el cerebro, lo que se conoce como accidente cerebrovascular hemorrágico.
Con frecuencia, la ruptura de un aneurisma cerebral se produce en el espacio entre el cerebro y los tejidos delgados que lo recubren. Este tipo de accidente cerebrovascular hemorrágico se denomina hemorragia subaracnoidea.
Los aneurismas cerebrales son comunes, pero la mayoría de ellos no son graves, en especial si son pequeños. La mayor parte de los aneurismas cerebrales no se rompen. No suelen producir síntomas ni causar problemas de salud. En muchas ocasiones, los aneurismas cerebrales se detectan cuando se hacen pruebas por otras afecciones.
Sin embargo, la ruptura de un aneurisma pone en riesgo la vida rápidamente y requiere tratamiento médico inmediato.
Si el aneurisma cerebral no se ha roto, el tratamiento puede ser adecuado en algunos casos. El tratamiento de un aneurisma intacto puede evitar una ruptura en el futuro. Habla con el proveedor de atención médica para asegurarte de conocer las mejores opciones para tus necesidades específicas.
Tipos
Aneurismas cerebrales saculares y fusiformes
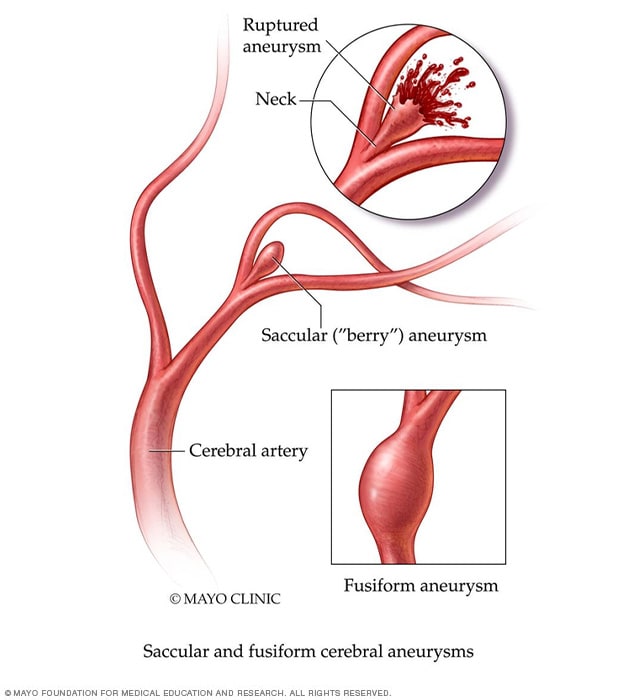
Aneurismas cerebrales saculares y fusiformes
El aneurisma sacular se conoce como aneurisma en baya. Es el tipo más común de aneurisma cerebral. Parece una baya colgando de una enredadera. Otro tipo de aneurisma es el aneurisma fusiforme. Provoca el abombamiento o la dilatación de la arteria.
- Aneurisma sacular, o aneurisma en baya. Este tipo de aneurisma parece una baya colgando de una enredadera. Es un saco redondo lleno de sangre que sobresale de la arteria principal o una de sus ramas. Generalmente, se forma en las arterias en la base del cerebro. El aneurisma en baya es el tipo más común de aneurisma.
- Aneurisma fusiforme. Este tipo de aneurisma causa un abultamiento en todos los lados de la arteria.
- Aneurisma micótico. Este tipo de aneurisma es ocasionado por una infección. Cuando una infección afecta las arterias del cerebro, puede debilitar la pared arterial. Esto puede causar que se forme un aneurisma.
Productos y servicios
Síntomas
La mayoría de los aneurismas que permanecen intactos no causan síntomas. Sobre todo si son pequeños. Los aneurismas cerebrales pueden detectarse en las pruebas por imágenes que se hacen por otras afecciones.
Sin embargo, la ruptura de un aneurisma es una afección muy grave, que generalmente causa un dolor de cabeza intenso. Y si un aneurisma intacto presiona los nervios o el tejido del cerebro, puede causar dolor y otros síntomas.
Rotura de un aneurisma
Un dolor de cabeza repentino e intenso es el síntoma clave de la ruptura de un aneurisma. Este dolor de cabeza suele describirse como el peor dolor de cabeza que puedas sentir.
Además de un dolor de cabeza intenso, los síntomas de la ruptura de un aneurisma pueden incluir lo siguiente:
- Náuseas y vómitos
- Rigidez en el cuello
- Visión borrosa o visión doble
- Sensibilidad a la luz
- Convulsiones
- Caída del párpado
- Pérdida del conocimiento
- Desorientación
Aneurisma con filtración
En algunos casos, un aneurisma puede filtrar una pequeña cantidad de sangre. Cuando esto ocurre, suele producirse una ruptura más grave. Las filtraciones pueden producirse días o semanas antes de la rotura.
Entre los síntomas de un aneurisma cerebral con filtraciones se pueden incluir los siguientes:
- Un dolor de cabeza repentino y muy intenso que puede durar varios días y hasta dos semanas.
Aneurisma sin rotura
Un aneurisma cerebral intacto puede no producir síntomas, especialmente si es pequeño. Sin embargo, un aneurisma intacto de mayor tamaño puede presionar los tejidos y nervios cerebrales.
Los síntomas de un aneurisma cerebral intacto pueden ser:
- Dolor en la parte superior y posterior de un ojo.
- Una pupila dilatada.
- Un cambio en la visión o visión doble.
- Entumecimiento en un lado de la cara.
Cuándo consultar al médico
Busca atención médica inmediata si tienes lo siguiente:
- Dolor de cabeza repentino y muy intenso
Si estás con alguien que se queja de un dolor de cabeza repentino e intenso, que pierde el conocimiento o que tiene una convulsión, llama al 911 o al número local de emergencias.
Mayo Clinic Minute: ¿Qué es un aneurisma?
Vivien Williams: ”Un aneurisma es una protrusión o un abombamiento anormal en las paredes de un vaso sanguíneo”.
Dr. Bernard Bendok, Neurocirugía, Mayo Clinic: ”En una parte de estos pacientes se producirá una ruptura, y el problema con las rupturas es que son impredecibles”.
Vivien Williams: ”El Dr. Bernard Bendok afirma que la ruptura de un aneurisma es una emergencia médica que puede causar un sangrado mortal en el cerebro”.
Dr. Bendok: ”La presentación típica es la de alguien que tiene el peor dolor de cabeza de su vida”.
Vivien Williams: ”Es esencial tratarlo rápidamente. Esto incluye cirugía abierta u otras opciones menos invasivas, como sellar la arteria rota desde dentro del vaso sanguíneo con espirales de metal o estents.
El Dr. Bendok dice que entre el 1 % y el 2 % de la población tiene aneurismas y solo un pequeño porcentaje de ese grupo presentará una ruptura. Las personas que tienen antecedentes familiares de aneurismas, enfermedad renal poliquística, enfermedad del tejido conectivo y quienes fuman tienen más riesgo de ruptura y deben considerar la posibilidad de someterse a exámenes de detección. Cuando se produce una ruptura, el tratamiento rápido salva la vida.
Soy Vivien Williams para la Red Informativa de Mayo Clinic”.
Causas
La causa de los aneurismas cerebrales es el afinamiento de las paredes de las arterias. Los aneurismas suelen formarse en las bifurcaciones o ramas de las arterias porque esas zonas de los vasos sanguíneos son más débiles. Si bien los aneurismas pueden aparecer en cualquier lugar del cerebro, son más comunes en las arterias que se encuentran en la base de este.
Factores de riesgo
Varios factores pueden contribuir a debilitar la pared arterial. Estos factores pueden aumentar el riesgo de tener un aneurisma cerebral o su ruptura.
Algunos de estos factores de riesgo se desarrollan con el tiempo. Pero algunas afecciones presentes en el nacimiento pueden aumentar el riesgo de tener un aneurisma cerebral.
Los factores de riesgo incluyen los siguientes:
- Edad avanzada. Los aneurismas cerebrales pueden ocurrir a cualquier edad. Sin embargo, son más frecuentes en los adultos de entre 30 y 60 años.
- Sexo femenino. Los aneurismas cerebrales son más comunes en las mujeres que en los hombres.
- Fumar cigarrillos. Fumar es un factor de riesgo para la formación de aneurismas cerebrales y su ruptura.
- Presión arterial alta. Esta afección puede debilitar las arterias. Es más probable que se formen aneurismas, y que se rompan, si tienes arterias debilitadas.
- Consumo de drogas ilícitas, especialmente cocaína. El consumo de drogas ilícitas aumenta la presión arterial. Si se administran por vía intravenosa, puede producirse una infección, que, a su vez, puede derivar en un aneurisma micótico.
- Consumo excesivo de alcohol. Esto también puede aumentar la presión arterial.
- Trastornos hereditarios del tejido conectivo, como el síndrome de Ehlers-Danlos. Estos trastornos debilitan los vasos sanguíneos.
- Enfermedad renal poliquística. Este trastorno hereditario ocasiona la formación de sacos llenos de líquido en los riñones. También puede aumentar la presión arterial.
- Estrechamiento de la aorta, denominado coartación aórtica. La aorta es el vaso sanguíneo grande que transporta sangre rica en oxígeno desde el corazón al cuerpo.
- Malformación arteriovenosa cerebral. En esta afección, las venas y arterias del cerebro están enredadas. Esto afecta el flujo sanguíneo.
- Antecedentes familiares de aneurismas cerebrales. Tu riesgo aumenta si tienes familiares que hayan tenido un aneurisma cerebral. Esto es particularmente cierto si dos o más familiares de primer grado, como padre, madre, hermano, hermana, hijo o hija, han tenido un aneurisma cerebral. Si tienes antecedentes familiares, puedes consultar al proveedor de atención médica sobre las pruebas de detección de aneurismas cerebrales.
Es posible que algunos tipos de aneurismas aparezcan después de una lesión en la cabeza o a partir de ciertas infecciones en la sangre.
Factores de riesgo para la ruptura de un aneurisma
Existen algunos factores que aumentan las probabilidades de que un aneurisma se rompa. Entre estos, se incluyen los siguientes:
- Tener un aneurisma grande.
- Tener aneurismas en determinadas zonas.
- Fumar cigarrillos.
- No recibir tratamiento para la presión arterial alta.
Complicaciones
Cuando se rompe un aneurisma cerebral, el sangrado suele durar solo unos segundos. Sin embargo, la sangre puede ocasionar daño directo a las células circundantes y matar neuronas cerebrales. También aumenta la presión en el interior del cráneo.
Si la presión aumenta mucho, el suministro de sangre y oxígeno al cerebro puede interrumpirse. Puede ocurrir pérdida del conocimiento o incluso la muerte.
Entre las complicaciones que pueden presentarse después de la ruptura de un aneurisma, se incluyen las siguientes:
- Nuevo sangrado. Un aneurisma que se rompió o se perforó corre el riesgo de volver a sangrar. El nuevo sangrado puede causar más daño a las neuronas cerebrales.
- Estrechamiento de los vasos sanguíneos del cerebro. Después de que se rompe un aneurisma cerebral, los vasos sanguíneos del cerebro pueden contraerse y estrecharse. Esto se conoce como vasoespasmo. Los vasoespasmos pueden causar un accidente cerebrovascular isquémico, en el que hay un flujo sanguíneo limitado hacia las neuronas cerebrales. Esto puede causar daño y pérdida adicionales de células.
- Acumulación de líquido en el interior del cerebro, conocido como hidrocefalia. Con frecuencia, la ruptura de un aneurisma cerebral se produce en el espacio entre el cerebro y los tejidos delgados que lo recubren. La sangre puede bloquear el movimiento del líquido que rodea el cerebro y la médula espinal. Como consecuencia, el exceso de líquido ejerce presión en el cerebro y puede dañar los tejidos.
- Cambios en el nivel de sodio. El sangrado en el cerebro puede interrumpir el equilibrio de sodio en la sangre. Esto puede deberse al daño en el hipotálamo, una zona que se encuentra cerca de la base del cerebro. La disminución de los niveles de sodio en la sangre puede derivar en la hinchazón de las neuronas cerebrales y en daños permanentes.
Prevención
En muchos casos, los aneurismas cerebrales no pueden prevenirse. Pero hay algunos cambios que puedes hacer para reducir el riesgo. Estos incluyen dejar de fumar si lo haces. También es aconsejable trabajar con el proveedor de atención médica para bajar la presión arterial si es elevada. No bebas grandes cantidades de alcohol ni consumas drogas ilícitas como la cocaína.