Diagnosis
Liver biopsy

Liver biopsy
A liver biopsy removes a small sample of liver tissue for lab testing. A liver biopsy most often is done by putting a thin needle through the skin and into the liver.
Diagnosing Wilson's disease can be hard because its symptoms are similar to those of other liver diseases, such as hepatitis. Symptoms also may appear slowly over time. Changes in behavior that come on gradually can be especially hard to link to Wilson's disease.
Diagnostic criteria
Healthcare professionals diagnose Wilson's disease based on a combination of symptoms, lab values, and imaging or genetic tests. A structured scoring tool, such as the Leipzig diagnostic criteria, can help healthcare professionals combine these symptoms and test results to confirm or rule out Wilson's disease. The tool assigns points based on symptoms and test results. A Leipzig score of 4 or higher, for example, means Wilson's disease is highly likely.
Tests and procedures may include:
Blood and urine tests
Blood tests can show how well your liver is working and measure ceruloplasmin, a protein that binds copper in the blood. Blood tests also can check the level of copper in your blood. Your healthcare professional may want to measure the amount of copper removed in your urine during a 24-hour period.
- Ceruloplasmin. This test checks the levels of a protein that binds copper in the blood. In Wilson's disease, ceruloplasmin levels are typically low. What is considered low depends on the specific laboratory, but below 20 milligrams per deciliter (mg/dL) or 0.2 grams per liter (g/L) is often considered low. The levels are low because the ATP7B gene change that causes Wilson's disease prevents copper from binding properly to ceruloplasmin protein. Some people with Wilson's disease do not have low ceruloplasmin levels. And you can have low ceruloplasmin levels without having Wilson's disease. For example, liver disease caused by something else may lower ceruloplasmin levels.
- Serum copper. This test checks the level of copper in blood. By itself, the test is not used to diagnose Wilson's disease. With Wilson's disease, total serum copper levels usually are low due to low ceruloplasmin. However, the level of free copper — copper that isn't bound to ceruloplasmin — is often higher than usual.
- 24-hour urinary copper. Your healthcare professional may want to measure the amount of copper removed in your urine during a 24-hour period. With Wilson's disease, this level is typically high. What is considered high depends on the specific laboratory, but higher than 40 to 100 micrograms (mcg) a day usually is considered high.
- Other liver tests. Other tests might be done to check how well your liver is working. These are called liver function tests. But Wilson's disease can cause liver damage with normal liver function and normal test results. This is called compensated liver disease.
Eye exam
During an eye exam, an eye specialist can use a special light called a slit-lamp to check for Kayser-Fleischer rings and sunflower cataracts.
Kayser-Fleischer rings are golden-brown or copper-colored and appear around the outside edge of the colored part of the eye, called the iris. The rings are caused by copper buildup in a part of the cornea called the Descemet membrane. The cornea is the clear, dome-shaped layer that covers the pupil and iris. Kayser-Fleischer rings are seen in most people with neurological symptoms and about half of people with symptoms of liver disease only.
Wilson's disease also can cause a special kind of cataract, called a sunflower cataract. This is caused by copper buildup in the lens of the eye.
Liver biopsy
In a liver biopsy, a healthcare professional inserts a thin needle through your skin and into your liver to take a small sample of tissue. A laboratory then tests the tissue for extra copper. A copper level higher than 250 micrograms per gram of dry weight liver (mcg/g) is a sign of Wilson's disease.
Genetic testing
A blood test can look for mutations in the ATP7B gene, which is what causes Wilson's disease. There are hundreds of known mutations in the ATP7B gene. One of the most common is p.H1069Q. If you have the changed gene that causes Wilson's disease, any siblings and children should get genetic testing too. Finding the condition early means they can begin treatment before symptoms start.
MRI
Magnetic resonance imaging (MRI) is a medical imaging technique that uses a magnetic field and computer-generated radio waves to create detailed images of organs and tissues in the body. In those with neurological symptoms of Wilson's disease, a brain MRI may show changes in parts of the brain affected by copper buildup. The face of the giant panda sign appears on a brain MRI in about 10% to 15% of people with Wilson's disease. It shows when Wilson's disease has damaged the middle part of the brain called the midbrain. The name of the sign reflects a pattern of lighter and darker colors that look similar to a panda's face in the MRI image.
Conditions that may have similar symptoms
When diagnosing Wilson's disease, healthcare professionals think about other possible conditions that might cause similar symptoms. This helps ensure the correct diagnosis and treatment.
All of these other conditions are caused by different gene changes:
- Hemochromatosis. Like Wilson's disease, hemochromatosis can affect the liver. But a difference between Wilson's disease and hemochromatosis is that Wilson's disease involves a buildup of copper. Hemochromatosis involves too much iron.
- Huntington's disease. Both Wilson's disease and Huntington's disease can cause similar movement and behavior symptoms. But Wilson's disease is different from Huntington's disease in that it affects both the liver and the brain due to copper buildup. Huntington's disease affects the brain by causing nerve cells in the brain to decay over time.
- Aceruloplasminemia. Aceruloplasminemia and Wilson's disease are not related, though both affect the ceruloplasmin protein that binds copper in the blood. Aceruloplasminemia leads to iron buildup, not copper buildup, in the liver.
- Menkes disease. Menkes disease also affects how the body uses copper. But Wilson's disease is not the same as Menkes disease. Menkes disease leads to a low level of copper in the liver and brain. Wilson's disease results in a high level of copper in the liver and brain.
- Other copper or iron metabolism conditions. A few other rare inherited conditions can affect copper and iron balance. But they have different genetic causes.
All of these conditions are caused by gene changes different from the gene change that causes Wilson's disease. And all have different effects on the body.
More Information
Treatment
To treat Wilson's disease, a healthcare professional may first recommend medicines called copper chelating agents. These medicines attach themselves to copper and cause the organs to release that copper into the bloodstream. The kidneys then filter the copper and release it into urine.
Treatment then focuses on stopping copper from building up again. This often is done with a zinc medicine. For severe liver damage, a liver transplant might be needed.
Can Wilson's disease be cured?
Treatment protects the body from further damage from Wilson's disease and can improve some symptoms. Medicines do not cure Wilson's disease. A liver transplant cannot cure the gene change that causes Wilson's disease. But a donated liver would not have the mutated gene, so it would process copper properly without more treatment. If Wilson's disease is detected early and treated, a person with the disease can live a full life and have a typical life expectancy.
Medicines
If you take medicines for Wilson's disease, you'll need to continue taking them for life, unless you have a liver transplant.
Chelating agents for copper removal
These medicines often are used first, as an initial treatment to lower copper levels quickly:
- Penicillamine (Cuprimine, Depen). Penicillamine, sometimes referred to as d-penicillamine, is a medicine that removes extra copper from the body. It can cause serious side effects, including skin and kidney issues. It also can cause or worsen neurological symptoms, most often in those who already have neurological symptoms. It also may lower the bone marrow's ability to make enough red blood cells and platelets. Use penicillamine carefully if you have a penicillin allergy. Because penicillamine reduces the effect of vitamin B6, also known as pyridoxine, you'll also need to take small doses of a B6 supplement.
- Trientine (Cuvrior, Syprine). This is another medicine that removes extra copper from the body. It works much like penicillamine but usually causes fewer side effects. Still, neurological symptoms can get worse when taking trientine.
Zinc therapy to prevent copper absorption
Zinc acetate (Galzin) stops your body from absorbing copper from the food you eat. This medicine usually is used as maintenance therapy to stop copper from building up again after initial treatment with penicillamine or trientine. Zinc acetate may be used as the main treatment if you can't take penicillamine or trientine or if you have no symptoms. The most common side effect of zinc acetate is stomach upset.
Your healthcare professional also might recommend ways to treat other symptoms of Wilson's disease.
Surgery
Living-donor liver transplant
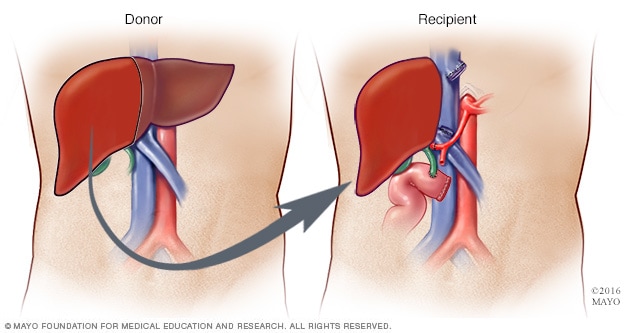
Living-donor liver transplant
During a living-donor liver transplant, surgeons remove about 40% to 70% of the donor liver and place it into the recipient.
If your liver is so damaged that you're in liver failure, or if the damage can't be reversed with medicine, you might need a liver transplant. During a liver transplant, a surgeon removes your damaged liver and replaces it with a healthy liver from a donor.
Most transplanted livers come from donors who have died. Sometimes a liver can come from a living donor, such as a family member. In that case, the surgeon removes your liver and replaces it with a portion of the donor's liver.
Lifestyle and home remedies
Wilson's disease is managed with lifelong medicine to remove and block extra copper in the body, along with self-care to be sure you don't have too much copper in your diet.
If you're told to limit copper in your diet, this may include copper found in water, supplements and food.
Water
If your home has copper pipes, run the water until it turns cool before using it for cooking or drinking. If you use well water, have it tested for copper, or use a filter that removes trace elements.
Supplements
Be sure to stay away from multivitamins or supplements that have copper.
Food
If you have Wilson's disease, talk to your healthcare team about how to adjust your diet to meet any needed dietary restrictions and dietary guidelines.
Your healthcare team will likely recommend that you limit copper. But how much is OK may depend on what stage of treatment you're in as well as other personal health factors. As an example, you might initially be asked to have no more than 1 milligram (mg) of copper per day. Later, on a maintenance plan, you might be told you can have a moderate amount of copper, such as 2 mg or less per day.
Foods that have high amounts of copper
If you have Wilson's disease, you may be asked to avoid or limit these foods:
- Liver and other organ meats.
- Shellfish and shrimp.
- Lamb.
- Goose, duck and quail.
- Tofu, soy protein and soy milk.
- Dried beans.
- Mushrooms.
- Sweet potatoes and other potatoes with skin.
- Dried fruits.
- Soy flour, bran cereals and corn grain.
- Nuts and seeds.
- Chocolate.
- Mineral water.
Foods that have low amounts of copper
Your healthcare team may tell you that you can eat more of these foods as a base of your diet if you have Wilson's disease:
- White meat chicken and turkey.
- Cod, scallops, halibut, tuna and trout.
- Eggs, butter and margarine.
- Cheese, cottage cheese and sour cream.
- Almond milk, cow's milk and yogurt, as long as they're not chocolate flavored.
- Brussels sprouts, broccoli and cabbage.
- Cauliflower, spinach and green peppers.
- Onions.
- Shiitake and enoki mushrooms.
- Apples, blueberries, cherries, plums, melons, strawberries and watermelon.
- Coffee and carbonated beverages.
Some healthy foods have a moderate level of copper and may be allowed in small amounts. Ask your healthcare team what dietary guidelines are OK for you.
It's common to have questions or worry about whether you can live a normal life with Wilson's disease. Starting lifelong medicine and learning new eating habits can feel like a lot to manage. Give yourself time to adjust, and share your concerns with your healthcare team. It also may help to know that with early diagnosis, proper medical treatment and self-care, most people with Wilson's disease live healthy lives.
Preparing for your appointment
You'll likely first see your primary healthcare professional. You may then be referred to a healthcare professional who specializes in the liver, called a hepatologist.
What you can do
When you make the appointment, ask if you need to do anything to prepare, such as change your diet before blood tests.
It may help to make a list of:
- Your symptoms and when they began.
- Important personal information, including major stresses, other health conditions and any family history of Wilson's disease.
- All medicines, vitamins or supplements you take, including the doses.
- Questions you want to ask your healthcare professional.
If possible, bring someone with you to help you remember the information you're given.
If you think you might have Wilson's disease or have been told you do, you may want to ask your healthcare professional questions such as:
- What tests do I need to confirm Wilson's disease?
- What family history details do you need?
- How is Wilson's disease treated and monitored long-term?
- What treatment do you recommend?
- What are the side effects of this treatment?
- How can I best manage Wilson's disease along with my other health conditions?
- Do I need to limit the types of food I eat?
- Should I see a specialist and, if so, what kind?
- Should my siblings or children be tested for Wilson's disease?
- What type of specialist should my family members see?
- Are there brochures or other printed materials that I can have? What websites do you recommend?
Be sure to ask any other questions you have. Also, be sure to tell your healthcare professional if anyone in your family has Wilson's disease or unexplained liver, neurological or mental health symptoms, since the disease runs in families.
What to expect from your doctor
Your healthcare professional may ask several questions such as:
- Do your symptoms occur all the time or do they come and go?
- How severe are your symptoms?
- How long have you had these symptoms?
- What, if anything, seems to make your symptoms better or worse?
- Does anyone else in your family have Wilson's disease?
Dec. 27, 2025