Diagnosis
Frontal lobe epilepsy can be hard to diagnose. Its symptoms can be mistaken for mental health problems or sleep disorders such as night terrors. It also is possible that some symptoms of frontal lobe seizures are the result of seizures that begin in other parts of the brain.
To make a diagnosis, a health care professional reviews your symptoms and medical history. The care professional also conducts a physical exam. You may have blood drawn to test for health conditions or disorders that may be causing the seizures.
You might need a neurological exam, which will test your:
- Muscle strength.
- Sensory skills.
- Hearing and speech.
- Vision.
- Coordination and balance.
You also might need the following tests:
-
Brain scans. Brain imaging — usually an MRI — might reveal the source of frontal lobe seizures. An MRI uses radio waves and a powerful magnetic field to produce detailed images of soft tissues, which make up the brain.
An MRI involves lying on a narrow table that slides into a long tube. The test often takes about an hour. Some people have a fear of enclosed spaces. They can be given a medicine to feel sleepy and less anxious. The test itself is painless.
- Electroencephalogram, known as an EEG. An EEG monitors the electrical activity in the brain. This is done by attaching small metal discs called electrodes to the scalp. EEGs often help diagnose some types of epilepsy. However, EEG results might not identify frontal lobe epilepsy.
- Video EEG. Video EEG is recommended for some people with seizures. This test is usually performed during an overnight stay at a sleep clinic. Both a video camera and an EEG monitor run all night. A video EEG allows health care professionals to match what physically occurs during a seizure with what appears on the EEG.
More Information
Treatment
Over the past decade, treatment options have increased for frontal lobe seizures. There are newer types of anti-seizure medicines. There also are a variety of surgical procedures that might help if medicines don't work.
Medications
All anti-seizure medicines seem to work equally well at controlling frontal lobe seizures. But not everyone becomes seizure-free on medicine. You may need to try different types of anti-seizure medicines. Or you may need to take a combination of medicines to control your seizures. Researchers are continuing to look for new and more-effective medicines.
Surgery
Implanted vagus nerve stimulation
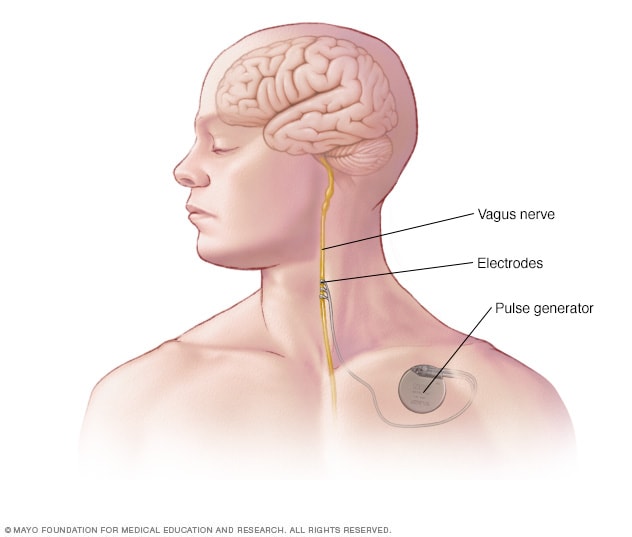
Implanted vagus nerve stimulation
In vagus nerve stimulation, a device placed under the skin of the chest stimulates the vagus nerve in the neck. This sends signals to the brain that lessen seizures.
If your seizures can't be controlled with medicines, surgery might be an option. Before surgery, the goal is to find the areas of the brain where seizures occur.
Imaging techniques can help identify the area generating seizures. These include single-photon emission computerized tomography (SPECT) and subtraction ictal SPECT coregistered to MRI (SISCOM).
Another imaging technique, known as brain mapping, is commonly used before epilepsy surgery. Brain mapping involves implanting electrodes into an area of the brain. Then electrical stimulation is used to determine whether that area has an important function. This helps to rule out surgery on certain areas of the brain. Functional MRI (fMRI), in particular, is used to map the language area of the brain.
If you have surgery for frontal lobe seizures, it's likely you'll need anti-seizure medicine after the surgery. But surgery may allow you to take a lower dose.
Deep brain stimulation
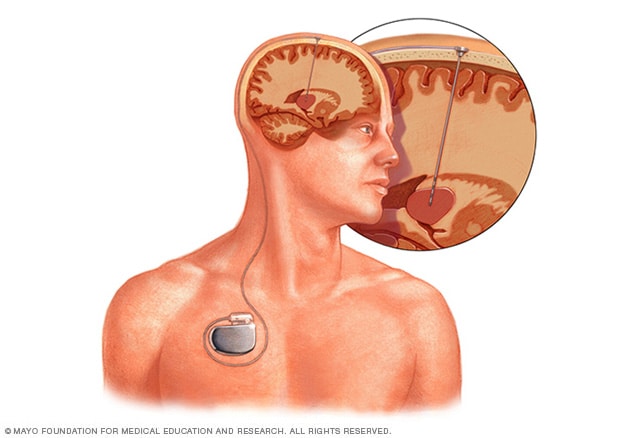
Deep brain stimulation
Deep brain stimulation involves putting an electrode deep within the brain. The amount of stimulation delivered by the electrode is controlled by a device placed under the skin in the chest. A wire that travels under the skin connects the device to the electrode.
Surgery for epilepsy might involve:
- Removing the focal point. If your seizures always begin in one spot in your brain, surgery removes that small portion of brain tissue. This might reduce the number of seizures you have. Or it might stop your seizures.
- Isolating the focal point. Sometimes the portion of the brain that's causing seizures is too vital to remove. When this happens, surgeons might make a series of cuts to help isolate that section of the brain. This prevents seizures from moving into other parts of the brain.
- Stimulating the vagus nerve. This involves implanting a device that's similar to a cardiac pacemaker, but it stimulates your vagus nerve. This procedure usually lowers the number of seizures you have.
- Responding to a seizure. A responsive neurostimulator is a newer type of implanted device. It is activated only when you begin to have a seizure. Once activated, it stops the seizure from occurring.
- Deep brain stimulation (DBS). This newer procedure involves implanting an electrode into your brain. The electrode is connected to a stimulating device under the skin of the chest. The device sends signals to the electrode in the brain to stop the activity that triggers a seizure.
Lifestyle and home remedies
You may find that some things trigger seizures. Seizures can be triggered by alcohol intake, smoking and, especially, lack of sleep. There also is evidence that severe stress can provoke seizures, and that seizures themselves can cause stress. Avoiding these triggers where possible might help improve seizure control.
Alternative medicine
Some people with neurological conditions, including seizures, turn to complementary and alternative medicine, such as:
- Herbs.
- Acupuncture.
- Psychotherapy.
- Mind-body techniques.
- Homeopathy.
Researchers are looking into these therapies to determine their safety and effectiveness. However, good evidence that they're effective at reducing seizures is mostly still lacking. There is some evidence that a ketogenic diet might be effective for treating seizures, particularly in children. A ketogenic diet is a strict high-fat, low-carbohydrate diet.
Many people with epilepsy use herbs to try to reduce their seizures. However, there's not enough evidence that most herbs are effective. Some herbs can cause an increased risk of seizures.
Marijuana, also known as cannabis, is one of the most commonly used herbs for treating epilepsy. The Food and Drug Administration (FDA) has approved a medicine that contains the purified marijuana chemical cannabidiol (Epidiolex). The medicine was approved to treat two rare forms of severe childhood epilepsy, Dravet syndrome and Lennox-Gastaut syndrome. Cannabidiol, also known as CBD, hasn't been approved in the United States or for any other types of epilepsy.
Researchers are studying how effective CBD may be for treating other types of seizures. They're also studying its potential risks, including how CBD interacts with anti-seizure medicines. Cannabis products have been reported to make seizures worse.
The FDA doesn't currently regulate herbal products. Herbs can interact with anti-seizure medicines, putting your health at risk. Talk to a health care professional before taking herbal or dietary supplements for your seizures.
Coping and support
Some people who have epilepsy are frustrated by their condition. Frontal lobe seizures can involve loud utterances or sexual movements that may make the person with epilepsy anxious.
Parents of children with frontal lobe seizures can find information, resources and emotional connections from support groups. Support groups also can help children who have epilepsy. Counseling also can be important. Adults with epilepsy can find support through in-person and online groups.
Preparing for your appointment
You're likely to first see a health care professional. This person may refer you to a doctor trained in nervous system conditions, called a neurologist.
What you can do
Ask a family member or friend to come with you to the appointment to help you remember the information you receive.
Make a list of:
- Your symptoms. Include even those that seem unrelated to the reason you scheduled the appointment, when they began and how often they occur.
- All medicines, vitamins and supplements you take, including doses.
- Questions to ask the health care professional.
Some questions to ask include:
- What is likely causing my symptoms or condition?
- Will I likely have more seizures? Will I have different types of seizures?
- What tests do I need? Do they require any special preparation?
- What treatments are available, and which do you recommend?
- I have other medical problems. How can I manage them together?
- Is surgery a possibility?
- Will I have restrictions on my activity? Will I be able to drive?
- Are there brochures or other printed materials I can have? What websites do you recommend?
What to expect from your doctor
You're likely to be asked questions, such as:
- Did you notice any unusual sensations before the seizures?
- How often do the seizures occur?
- Can you describe a typical seizure?
- How long do the seizures last?
- Do the seizures occur in clusters?
- Do they all look the same or are there different seizure behaviors you or others have seen?
- Have you noticed seizure triggers, such as illness or lack of sleep?
- Has anyone in your immediate family ever had seizures?
Sept. 19, 2023