Diagnosis
To diagnose aortic valve disease, a health care professional examines you and asks questions about your symptoms and medical history.
A whooshing sound, called a heart murmur, may be heard when listening to the heart with a stethoscope. If so, you may need to see a doctor trained in heart diseases, called a cardiologist.
Tests
Tests to diagnose aortic valve disease include:
Echocardiogram. An echocardiogram uses sound waves to create pictures of the beating heart. It shows how blood flows through the heart and heart valves. It can help determine the severity of aortic valve disease.
There are different types of echocardiograms. The type you have depends on the information your health care team needs. A standard echocardiogram is done from outside the body. The ultrasound device is gently pressed against the skin of the chest above the heart. If more details are needed about the heart, a transesophageal echocardiogram may be done. This type creates pictures of the heart from inside the body. The ultrasound device is attached to a tube that goes down your throat and into the esophagus.
- Electrocardiogram (ECG or EKG). This quick test records the electrical activity of the heart. It shows how the heart beats. Sticky patches are placed on the chest and sometimes the legs. Wires connect the patches to a computer, which displays or prints results.
- Chest X-ray. A chest X-ray shows the condition of the heart and lungs. It can help determine if the heart is enlarged, which can be a sign of certain types of aortic valve disease or heart failure.
- Cardiac MRI. A cardiac MRI uses magnetic fields and radio waves to create detailed pictures of the heart. This test may be used to determine the severity of aortic valve disease and measure the size of the aorta.
- Cardiac computerized tomography (CT) scan. A cardiac CT scan uses a series of X-rays to create detailed images of the heart and heart valves. The test may be done to measure the size of the aorta and look at the aortic valve more closely. A CT scan also may be used to measure the amount of calcium in the aortic valve or determine the severity of aortic valve stenosis.
- Exercise tests or stress tests. These tests often involve walking on a treadmill or riding a stationary bike while an ECG or echocardiogram is done. Exercise tests show how the heart reacts to physical activity and whether valve disease symptoms occur during exercise. If you can't exercise, you may get medicine that affects the heart like exercise does.
- Cardiac catheterization. This test isn't often used to diagnose aortic valve disease. But it may be done to see how severe aortic valve disease is or to diagnose the condition if other tests can't. In this test, a thin, flexible tube is inserted into a blood vessel, usually in the groin area or arm, and guided to the heart. Cardiac catheterization can give more details about blood flow and how well the heart is working. Certain heart treatments can be done during cardiac catheterization.
Staging
After testing confirms a diagnosis of aortic or other heart valve disease, your health care team may tell you the stage of disease. Staging helps determine the most appropriate treatment.
The stage of heart valve disease depends on many things, including symptoms, disease severity, the structure of the valve or valves, and blood flow through the heart and lungs.
Heart valve disease is staged into four basic groups:
- Stage A: At risk. Risk factors for heart valve disease are present.
- Stage B: Progressive. Valve disease is mild or moderate. There are no heart valve symptoms.
- Stage C: Asymptomatic severe. There are no heart valve symptoms but the valve disease is severe.
- Stage D: Symptomatic severe. Heart valve disease is severe and is causing symptoms.
Treatment
Treatment for aortic valve disease depends on:
- The severity (stage) of aortic valve disease.
- Whether the disease is causing symptoms.
- Whether the condition is getting worse.
Treatment may include regular health checkups, lifestyle changes, medicines, or surgery or other procedures. If you have aortic valve disease, consider being evaluated and treated at a medical center with a multidisciplinary team of heart doctors called cardiologists and other care professionals trained and experienced in evaluating and treating heart valve disease.
Medications
If aortic valve disease is mild or moderate or if you aren't having symptoms, you may only need regular medical checkups to watch the condition.
Heart-healthy lifestyle changes and medicines may be needed to treat symptoms of aortic valve disease or reduce the risk of complications. For example, medicines may be used to:
- Lower blood pressure.
- Prevent irregular heartbeats.
- Remove excess fluid from the body to reduce the strain on the heart.
Surgery or other procedures
Eventually, surgery or a catheter procedure may be needed to repair or replace the diseased aortic valve. Some people with aortic valve disease need surgery even if it's not severe or when it's not causing symptoms.
Surgery to repair or replace an aortic valve is often done with open-heart surgery. Sometimes, the valve can be replaced during minimally invasive heart surgery, which uses smaller incisions than those needed for open-heart surgery, or with a catheter-based procedure.
Aortic valve repair
During aortic valve repair, the surgeon may do one or all of the following:
- Separate valve flaps that have fused.
- Add support to the base of the valve.
- Reshape or remove excess valve tissue so that the cusps can close tightly.
- Patch holes or tears in a valve.
Aortic valve repair often requires open-heart surgery. However, less invasive options may be available. For example, a catheter procedure may be used to insert a plug or device to repair a leaking replacement aortic valve.
In infants and children with aortic valve stenosis, a less invasive procedure called balloon valvuloplasty may be done to temporarily open a narrowed valve. During this procedure, the doctor inserts a thin, hollow tube into a blood vessel, usually in the groin, and threads it to the heart. A balloon is inflated to widen the valve opening. Then the balloon is deflated and removed. This valve repair procedure also may be done in adults who are too sick for surgery or who are waiting for a valve replacement.
Aortic valve replacement
Mechanical valve replacement
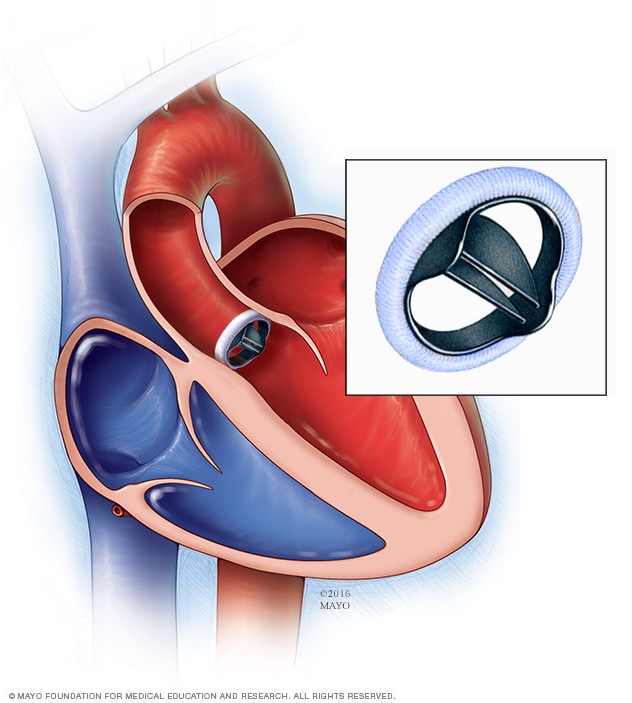
Mechanical valve replacement
In a mechanical valve replacement, an artificial heart valve made of strong material replaces the damaged valve.
Biological valve replacement
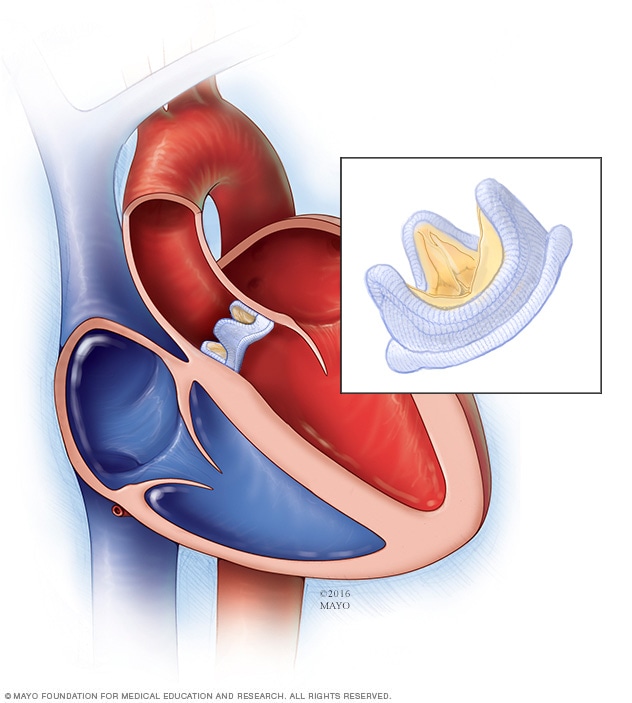
Biological valve replacement
In a biological valve replacement, a valve made from cow, pig or human heart tissue replaces the damaged heart valve.
Transcatheter aortic valve replacement (TAVR)
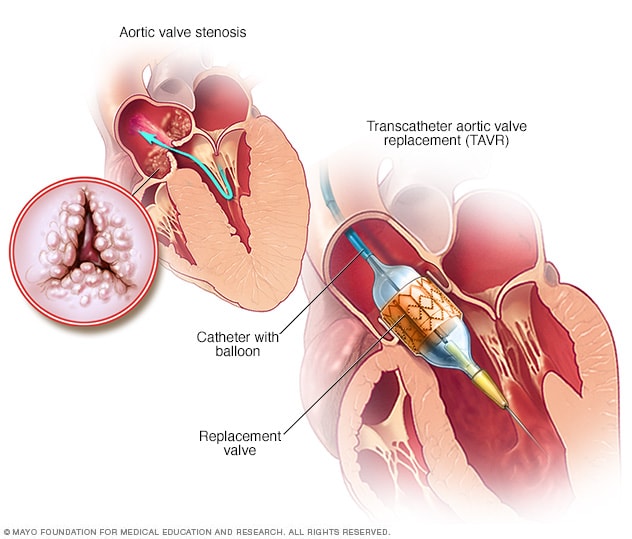
Transcatheter aortic valve replacement (TAVR)
Transcatheter aortic valve replacement, also called TAVR, is a type of heart valve surgery. It's done to replace a narrowed aortic valve. This is a condition called aortic valve stenosis. A doctor inserts a flexible tube called a catheter into a blood vessel and guides it into the heart. A replacement valve made of cow or pig tissue goes through the tube to the specific area in the heart. A balloon on the catheter tip inflates to press the new valve into place. Some valves expand on their own.
In aortic valve replacement, a surgeon removes the damaged valve and replaces it with a mechanical valve or a valve made from cow, pig or human heart tissue. A tissue valve is called a biological tissue valve.
Sometimes, the aortic valve is replaced with your own lung valve, called a pulmonary valve. Then your pulmonary valve is replaced with a biological lung tissue valve. This more complicated surgery is called the Ross procedure.
You and your health care team will discuss the benefits and risks of each type of valve to choose the best option for you.
Aortic valve replacement typically requires open-heart surgery. Sometimes, surgeons can use a minimally invasive procedure called transcatheter aortic valve replacement (TAVR) to replace a narrowed aortic valve with a biological tissue valve. TAVR uses smaller incisions than those used in open-heart surgery. TAVR may be an option for people at increased risk of heart valve surgery complications.
More Information
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
After diagnosis or treatment of aortic valve disease, you'll need regular health checkups. Your health care team may suggest making heart-healthy lifestyle changes. Try these steps:
- Eat a heart-healthy diet. Eat a variety of fruits and vegetables, low-fat or fat-free dairy products, poultry, fish, and whole grains. Avoid saturated and trans fats and excess salt and sugar.
- Maintain a healthy weight. Ask your health care team what a healthy weight is for you.
- Get regular exercise. As a general goal, aim for at least 30 minutes of moderate physical activity every day. Check with your health care team before starting a new exercise routine.
- Manage stress. Find ways to help reduce emotional stress. Getting more exercise, practicing mindfulness and connecting with others in support groups are some ways to tame stress.
- Do not smoke. If you need help quitting smoking or using tobacco, ask a health care professional about resources to help. Joining a support group may be helpful.
Pregnancy
If you have aortic valve disease, it's important to talk with a health care professional before becoming pregnant. Careful and regular checkups are needed if you have aortic valve disease during pregnancy. Your health care team can discuss with you which medicines are safe to use during pregnancy. Your health care team also can determine whether valve disease treatment is needed prior to pregnancy.
Health care professionals may recommend that people with severe heart valve disease avoid pregnancy to avoid the risk of complications.
Coping and support
If you have aortic valve disease, here are some steps that may help you manage the condition:
- Take medicines as prescribed. Take your medicines as directed by your health care team.
- Get support. Connecting with others who have the same or a similar condition may be helpful. Ask your health care team about support groups in your area.
- Stay active. Regular exercise is one of the best ways to improve heart health. Ask a health care professional about how much and what types of physical activity are safe for you.
Preparing for your appointment
If you think you have aortic valve disease, make an appointment for a health checkup. Here's some information to help you prepare for your appointment.
- Be aware of pre-appointment restrictions. When you make the appointment, ask if there's anything you need to do beforehand.
- Write down your symptoms, including any that seem unrelated to heart valve disease.
- Write down important personal information, including a family history of heart disease, and any major stresses or recent life changes.
- Make a list of all medicines, vitamins and supplements you take. Include the dosages.
- Take a family member or friend along, if possible. Someone who goes with you can help you remember information you receive.
- Write down questions to ask your health care team.
For aortic valve disease, some basic questions to ask your health care team include:
- What is likely causing my symptoms or condition?
- What are other possible causes for my symptoms or condition?
- What tests will I need?
- What's the best treatment?
- What are the options to the primary treatment you're suggesting?
- I have other health conditions. How can I best manage them together?
- Are there restrictions I need to follow?
- Should I see a specialist?
- If I need surgery, which surgeon do you recommend for heart valve surgery?
- Is there a generic alternative to the medicine you're prescribing?
- Are there brochures or other printed material I can take with me? What websites do you recommend?
Don't hesitate to ask other questions you have.
What to expect from your doctor
Your health care team is likely to ask you many questions, including:
- When did your symptoms begin?
- Do you always have symptoms, or do the symptoms come and go?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
Sept. 27, 2023