June 21, 2025
For many people, vasectomy is a simple and effective form of permanent contraception. However, for a small percentage — estimated between 1% and 2% — the procedure leads to chronic discomfort known as post-vasectomy pain syndrome (PVPS). Patients with this condition often present to their primary healthcare professionals or urologists seeking answers to a life-disrupting problem that is poorly understood and often inadequately addressed.
At Mayo Clinic in Rochester, Minnesota, Sevann Helo, M.D., a fellowship-trained microsurgeon in Urology, is offering patients with PVPS a path toward relief through vasectomy reversal, a definitive surgical solution for a select group of patients with refractory symptoms.
Understanding PVPS
PVPS is defined as persistent or intermittent scrotal pain lasting more than three months after vasectomy. The pain may be localized to the testicle, epididymis or spermatic cord and is often exacerbated by physical activity, sexual stimulation or ejaculation. In some patients, PVPS severely reduces quality of life.
The etiology of PVPS is multifactorial and may include:
- Epididymal congestion due to backpressure.
- Chronic inflammation.
- Neuropathic changes.
- Granuloma formation at the vasectomy site.
Many patients initially try conservative treatments, including anti-inflammatories, antibiotics, scrotal support and even spermatic cord blocks. However, for a subset of patients with persistent pain despite conservative management, surgical intervention may be indicated.
Vasectomy reversal as a treatment for pain
 إعادة وصل القناة المنوية
إعادة وصل القناة المنوية
يعيد الجرَّاحون المجهريون التدفق الطبيعي ويخففون الضغط المتزايد في البربخ.
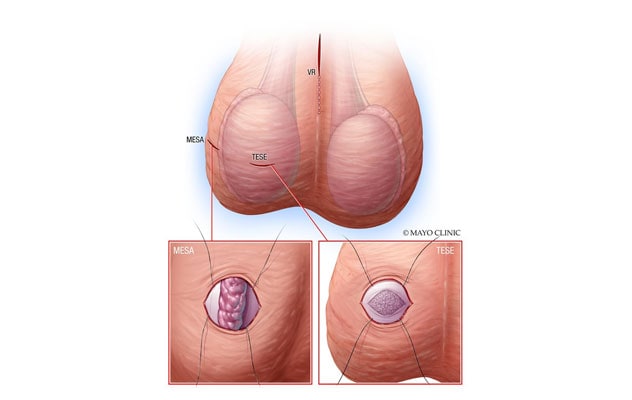
Vasectomy reversal is most discussed in the context of fertility restoration. However, in the hands of skilled microsurgeons, it is also an effective therapeutic option for PVPS, particularly in patients whose pain is believed to stem from epididymal distension or vasal obstruction.
"Vasectomy reversal works by reestablishing normal flow and relieving the pressure that builds up in the epididymis," explains Dr. Helo, who has established a specialized practice at Mayo Clinic focused on microsurgical reconstruction and male infertility.
Numerous studies have demonstrated that vasectomy reversal can significantly reduce or eliminate pain in 70% to 90% of carefully selected patients with PVPS, especially those who meet the following criteria:
- Focal epididymal tenderness on physical exam.
- Symptom onset directly linked to vasectomy.
- Absence of signs suggesting neuropathic pain or referred pain.
Dr. Helo's microsurgical expertise
Dr. Helo trained at Mayo Clinic and completed a fellowship in andrology and male infertility. Since joining Mayo Clinic, she has performed over 400 vasectomy reversals. She combines technical expertise with compassionate, patient-centered care to guide patients through what is often a deeply frustrating and emotionally complex diagnosis.
"Patients with post-vasectomy pain are often dismissed or told to live with it," says Dr. Helo. "My goal is to provide validation, a thorough workup and evidence-based options, including surgical ones when appropriate."
Using an operating microscope, Dr. Helo performs vasectomy reversals through a small incision with high magnification and precision. Patency rates in her hands are high, and the added benefit of performing procedures at a high-volume academic center allows for comprehensive evaluation and follow-up.
Mayo Clinic's multidisciplinary advantage
One of the unique strengths of Mayo Clinic is the integrated, team-based approach to complex conditions. Dr. Helo frequently collaborates with colleagues in pain medicine, radiology and psychology to evaluate patients holistically. Patients benefit from:
- Detailed imaging to rule out other sources of scrotal or pelvic pain.
- Nerve blocks to assess for neuropathic contribution.
- Psychological support when pain affects mood and relationships.
This multidisciplinary model helps ensure that surgical candidates are appropriately selected and supported throughout their care journeys.
Referral process and what to expect
Referring physicians can expect timely and collaborative communication. Dr. Helo accepts referrals for evaluation of:
- Post-vasectomy scrotal or testicular pain.
- Chronic orchialgia potentially linked to prior vasectomy.
- Reversal in patients seeking both pain relief and fertility restoration.
Initial consultations involve a detailed history, physical exam, review of prior imaging and operative reports, and for many patients, adjunct testing. If a patient is a candidate for vasectomy reversal, Dr. Helo provides education about the procedure, expected outcomes, recovery and potential risks.
Mayo Clinic offers:
- Streamlined scheduling for out-of-town patients.
- Concierge services to coordinate multidisciplinary evaluations.
- Access to world-class microsurgical equipment and facilities.
Outcomes and long-term care
Pain resolution after vasectomy reversal may occur immediately or gradually over several weeks to months. Most patients experience significant improvement in quality of life, with many able to return to sexual activity and physical exercise without discomfort.
Conclusion: A commitment to restoring quality of life
For patients with PVPS, Dr. Helo's practice at Mayo Clinic offers expert evaluation and a full range of treatment options — from conservative management to advanced microsurgical reversal. Her work is restoring comfort, confidence and hope to people whose lives have been impacted by this often-overlooked condition.
For more information
Refer a patient to Mayo Clinic.