June 21, 2019
Approximately 1% of men in the United States will be diagnosed with urethral stricture disease. This incidence increases with advancing age and can be attributed to urethral instrumentation for benign prostatic hyperplasia, cancer-related therapies and other comorbidities that adversely impact male urethral health, such as peripheral vascular disease and hypogonadism.
In a nationwide evaluation of board-certified urologist case logs published in Urology in 2015, only 4% of urethral stricture procedures performed were definitive urethroplasty. While the decision to pursue less invasive means to treat stricture disease is often multifactorial, evidence suggests that fellowship training in urethral reconstruction greatly lowers the ratio of endoscopic treatments relative to urethroplasty, from 25-to-1 to 10-to-1.
Urologist Boyd R. Viers, M.D., with Mayo Clinic in Rochester, Minnesota, says that this paradigm shift toward formal urethral reconstruction is likely the result of several recent advancements, including:
- Strong evidence for unintended consequences of repetitive endoscopic treatment
- An algorithmic pathway toward safe opioid prescribing habits and effective outpatient urethroplasty
- Implementation of robotic posterior urethral reconstruction for recalcitrant posterior urethral stenosis
Repetitive endoscopic treatments increase stricture complexity and risk of subsequent urethroplasty failure
Dr. Viers notes: "The recent American Urological Association urethral stricture guideline considers endoscopic management via dilation or internal urethrotomy a first line option for the initial treatment of short ― less than 2 cm ― bulbar urethral strictures. There has been a longstanding assumption that these maneuvers safely and effectively mitigate urethral stricture disease, thereby avoiding the need for risky surgical reconstruction. Unfortunately, the long-term success rate of endoscopic treatment has been poor (10% to 30%) and often commits these symptomatic patients to a repetitive cycle of temporizing urethral manipulations that delay definitive surgical therapy.
"It is now evident that even these minimally invasive methods are in fact associated with substantial unintended consequences, including a delay in definitive treatment, increased stricture complexity and risk of subsequent urethroplasty failure.
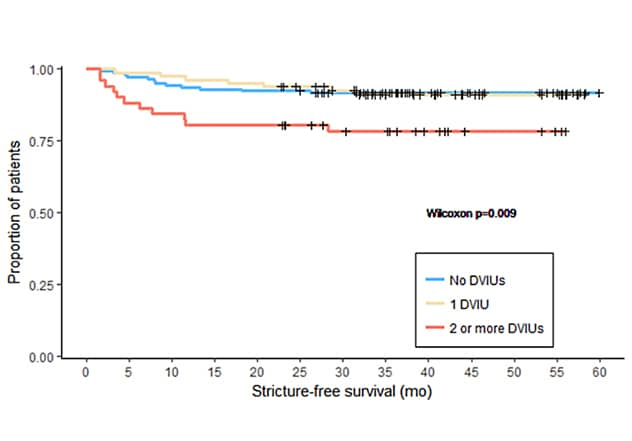
"In a consecutive series of 278 first-time bulbar urethroplasty cases, the median delay between stricture diagnosis and formal reconstruction was five years. During this time, patients required an average of one endoscopic procedure per year of delay.
شَق مجرى البول الداخلي (DVIU) بالمناظير، والنجاة من تضييق لرَأْب الإِحْليل البصلي التابع
شَق مجرى البول الداخلي (DVIU) بالمناظير، والنجاة من تضييق لرَأْب الإِحْليل البصلي التابع
ترتبط زيادة عدد مرات العلاجات بالمناظير بشكل مستقل بالتضييقات الأكثر طولًا التي تتطلب تنفيذ تقنيات ترميمية أكثر تعقيدًا. لقد كانت كل عملية شقِّ مجرى البول الداخلية (DVIU) مصحوبةً بزيادة ملحوظة بنسبة 19% في خطر الإصابة بفشل رَأْب الإِحْليل التابع.
"More importantly, a study published in the Journal of Urology in 2018 showed that increasing numbers of endoscopic treatments were independently associated with longer strictures ― more than 2 cm ― requiring more-complicated reconstructive techniques, and each internal urethrotomy was associated with a 19% increased risk of subsequent urethroplasty failure.
"As a result, we now emphasize early and aggressive urethroplasty, even for most elderly men and those with radiation-induced stricture disease. Early formal reconstruction affords the opportunity for improved quality of life, restoration of urinary function, and durable treatment success ― currently 85% to 95% at five years."
Outpatient urethroplasty and opioid stewardship: Ready for prime time?
مسار الرعاية غير القائم على المسكنات الأفيونية بعد جراحة الإحليل الأمامي
مسار الرعاية غير القائم على المسكنات الأفيونية بعد جراحة الإحليل الأمامي
أدت استراتيجيات الخوارزمية القائمة على البيانات للتحكم في الألم بعد العملية الجراحية إلى تطوير مسار الرعاية غير القائمة على المسكنات الأفيونية لإعادة بناء مجرى البول.
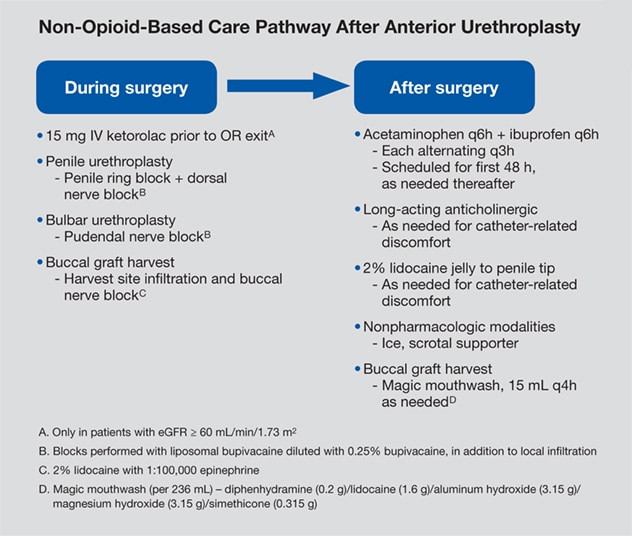
Traditionally, urethral reconstructive surgery often mandated several days of inpatient hospitalization and bed rest without any supporting evidence. At Mayo Clinic, approximately 80% of urethral reconstructive procedures have transitioned to an outpatient same-day ambulatory surgery. "With this approach, 95% of men report a high level of patient satisfaction and no difference in reconstructive outcomes," says Dr. Viers. "As we have made this transition to same-day surgery, we have been cognizant to develop data-driven algorithmic strategies for postoperative pain management. Through this evidence-based approach we have developed a non-opioid based care pathway for urethral reconstruction.
"Consequently, 75% of men without chronic opioid needs require less than five tablets of 5-mg oxycodone following major urethral reconstruction. In the face of an opioid epidemic where there has been significant effort to limit opioid prescribing habits among surgeons, this is one step toward reducing overprescribing and for many patients implementing opioid-free urethral surgery."
Robotic posterior urethral reconstruction for recalcitrant vesicourethral anastomotic stenosis
Reconstruction of the male posterior urethra in patients with vesicourethral anastomotic stenosis is one of the most challenging reconstructive surgeries performed by urologists. Obstacles encountered during this surgery include inadequate visualization, limited working space, and the scarred re-operative field. As a result, trepidation exists among urologists when considering formal reconstruction.
Dr. Viers notes: "As a consequence, the vast majority of men who develop post-prostatectomy anastomotic stenosis undergo lifelong temporizing management through some combination of intermittent self-dilation or endoscopic bladder neck dilation, incision or resection. Ultimately, many men may require chronic indwelling catheter drainage, which is associated with extremely poor quality of life.
"The overall impact of this surgical challenge is not inconsequential, given that 5% of men develop post-prostatectomy anastomotic stenosis, and each subsequent transurethral procedure, reflected in a recurrence rate of 33% at one year, is associated with increasing risk of stress incontinence, as supported by research published in European Urology Supplements in 2016.
"One of the traditional difficulties in this reconstruction is the combined transperineal and transabdominal approach. It requires transperineal exposure for urethral mobilization and transabdominal visualization for bladder neck dissection. Resection of the pubic bone is often necessary to achieve adequate visualization, tissue mobilization and a tension-free repair.
رَأْبُ الإِحْليل الخلفي الروبوتي
رَأْبُ الإِحْليل الخلفي الروبوتي
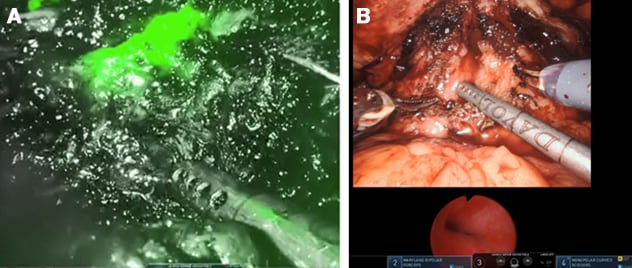
أ. تحدد تقنية أشعة الليزر تحت الحمراء الفلورية موقعَ ضِيقِ مجرى البول الخلفي بدقة. ب. الجمع بين التَّصْويرُ بالتَّنْظير المَثانِيِّ للجِهازِ البَولِيّ وباستخدام الروبوت الخاص بالعضلة العاصرة الغشائية للمثانة.
"Utilization of a robotic platform allows for enhanced optical magnification, infrared laser fluorescence technology to precisely identify stricture location and evaluate tissue integrity, and fine instrument manipulation enabling the surgeon to operate in the narrow confines of the male pelvis. For the majority of patients, this virtually eliminates the need for transperineal urethral mobilization and resection of the pubic bone. This simplified approach not only avoids additional morbidity but also preserves urethral integrity in the event the patient requires an artificial urinary sphincter.
"In general with a robot-assisted approach, patients who demonstrate sufficient external urinary sphincter function preoperatively are at a higher likelihood of maintaining urinary control following reconstruction ― a consequence of not violating the pelvic floor and external urinary sphincter complex as is done with a traditional combined abdominoperineal approach.
"Given the addition of this tool to our reconstructive armamentarium, we have redefined the way we think about treating vesicourethral anastomotic stenosis. In an effort to avoid damage to the urinary sphincter and expedite definitive care, we have implemented a stepwise approach in which the patient will undergo a single endoscopic treatment, preferably dilation, and if that fails, proceed to robotic reconstruction following a period of suprapubic tube with urethral rest."
For more information
Liu JS, et al. Practice patterns in the treatment of urethral stricture among American urologists: A paradigm change? Urology. 2015;86:830.
Viers BR, et al. Delayed reconstruction of bulbar urethral strictures is associated with multiple interventions, longer strictures and more complex repairs. Journal of Urology. 2018;199:515.
Viers BR, et al. Predictors of bladder neck contracture following radical prostatectomy. European Urology Supplements. 2016;15:e1018.