Jan. 19, 2021
Doctors at Mayo Clinic have been treating childhood and adolescent scoliosis for more than 75 years and see more than 700 children annually. Teams of pediatric specialists at Mayo Clinic Children's Center in Rochester, Minnesota, bring novel treatment approaches to children with scoliosis, from therapy and bracing to the latest in surgical techniques. Families can meet with care providers at Mayo Clinic's campus in Rochester, Minnesota, or in outreach clinics in North Dakota, Wisconsin, and the Minneapolis-St. Paul area of Minnesota. Video or telehealth visits also are available.
Nonfusion and guided growth techniques for scoliosis treatment
Mayo surgeons have sought to develop new treatment options for patients with scoliosis. "We heard from our patients that the traditional approach of fusion was not right for everyone, and we wanted to find a solution that would preserve motion and growth for our patients with scoliosis," says A. Noelle Larson, M.D., a pediatric orthopedic surgeon and chair of Community Orthopedic Surgery at Mayo Clinic in Rochester, Minnesota.
Until recently, the only definitive option for patients with moderate to severe scoliosis was fusion surgery. Although this procedure provides powerful scoliosis correction and has a 40-year track record in orthopedics, it involves placement of two metal rods and up to 20 screws through a large open incision and permanently reduces motion over the part of the spine with the curve.
إجراء ربط الجسم الفقري
إجراء ربط الجسم الفقري
في إجراء رباط الجسم الفقري، يُوضع الطفل على الجانب الأيسر وتُجرى شقوق بطول 2 سم في جدار الصدر للسماح بالتصوير الجراحي من خلال كاميرا صغيرة. تُوضع مسامير في كل فقرة على الجزء المقعر من العمود الفقري، ثم تُربط بكبل بلاستيكي. يُشد الكبل لتصحيح ما يقرب من 50% من جنف العمود الفقري. مع نمو الطفل، يمكن أن يحدث تصحيح إضافي بمرور الوقت.
Since 2015, Mayo Clinic has performed vertebral body tethering (VBT), allowing for curve correction while preserving motion and growth. The Mayo Clinic team uses a minimally invasive thoracoscopic surgical approach to place implants in the front of the spine to correct the scoliosis and promote ongoing improvement of the curvature as the child grows. Mayo Clinic was the first center in the U.S. to place the Tether system, the first nonfusion device approved by the Food and Drug Administration (FDA) for the treatment of pediatric scoliosis, and is one of the few centers in the world to routinely use CT-guided navigation for this approach.
نتائج جراحة الدمج وربط الجسم الفقري
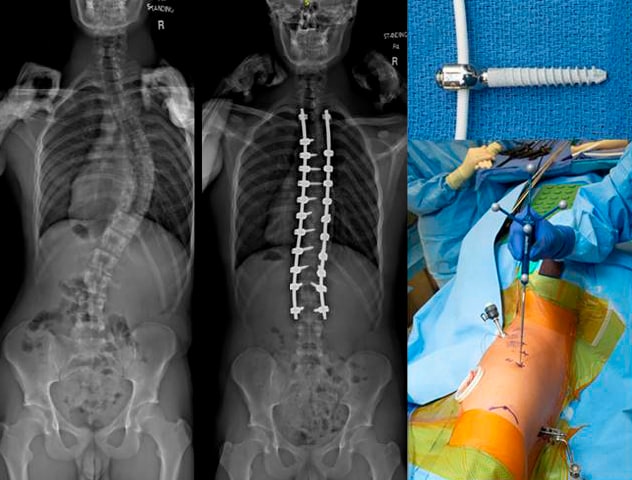
نتائج جراحة الدمج وربط الجسم الفقري
يسارًا. ينتج عن جراحة الدمج تصحيح ناجح ومتوقع للجنف، ولكن يؤدي إلى تقييد الحركة بسبب وضع دعامات معدنية قوية. وأيضًا كجزء من جراحة الدمج، تُزال المفاصل الوجيهية من على الجزء الخلفي من العمود الفقري. يمينًا. يتضمن ربط الجسم الفقري وضع مسامير التيتانيوم وحبل بلاستيكي مرن في الجزء الأمامي من العمود الفقري باستخدام تقنية منظار الصدر والتنقُّل الموجَّه بالتصوير المقطعي المحوسب.
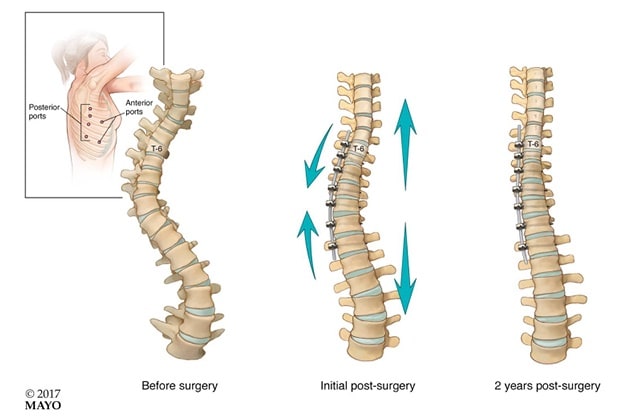
التقوس السابق للعملية الجراحية والتصحيح التالي لها

التقوس السابق للعملية الجراحية والتصحيح التالي لها
مثال على حالة، يوضح منحنى ما قبل الجراحة، والتصحيح الفوري بعد العملية الجراحية، والتصحيح المستمر بمرور الوقت مع نمو الطفل. يُؤمَّن نطاق حركي بزاوية 20 درجة تقريبًا من الوضع الأمامي إلى الخلفي و10 درجات تقريبًا من جانب إلى آخر بعد جراحة ربط الجسم الفقري، مع الحفاظ على التشريح الطبيعي للجسم.
"Instead of the rigid metal rods used for a fusion surgery, in VBT surgery a flexible cord is attached to each of the vertebrae and then tensioned, correcting the curve. This aligns the spine and gives vertebrae the needed space to grow properly," said Todd A. Milbrandt, M.D., an orthopedic surgeon and chair of Pediatric Orthopedics at Mayo Clinic in Rochester, Minnesota.
The procedure is designed to treat moderate to severe idiopathic scoliosis (measuring 40 to 65 degrees) and is recommended for children who are still growing. On average, boys complete their growth at age 16 and girls at 14, although there is significant variability. Compared with a fusion surgery, children typically return to sports more quickly and have less pain and fewer activity restrictions during the recovery period.
Posterior-based dynamic distraction device
التصوير السابق لعملية جراحة خلفية تعتمد على المباعدة.
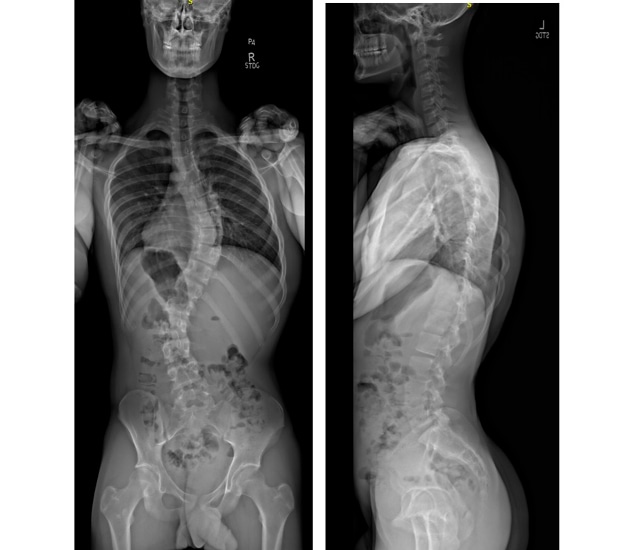
التصوير السابق لعملية جراحة خلفية تعتمد على المباعدة.
التصوير السابق للعملية لطفل خضع للعلاج بجراحة خلفية تعتمد على المباعدة.
التصوير التالي لعملية الجراحة الخلفية القائمة على المباعدة
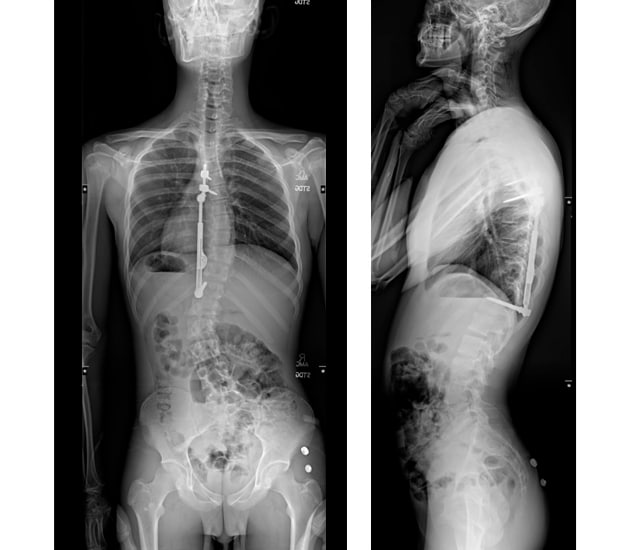
التصوير التالي لعملية الجراحة الخلفية القائمة على المباعدة
صورة مأخوذة بعد العملية الجراحية لطفل يُعالج بالجراحة الخلفية القائمة على المباعدة. على الرغم من أن التصحيح يصعب رؤيته بجراحة الالتحام التقليدية، إلا أن الجهاز يسمح بحركة العمود الفقري.
For patients with scoliosis who have completed their growth or who are only eligible for surgery from the back part of the spine, Mayo Clinic offers posterior distraction-based surgery. Mayo Clinic was the first in the U.S. to implant the FDA-approved Minimally Invasive Deformity Correction (MID-C) device. This system provides a nonfusion option for patients with flexible curves. It consists of a rod that has flexible joints and allows for some retained motion, in contrast to the solid rigid rod used for fusion surgery. This surgery may also have a faster recovery time than fusion.
"The MID-C device is placed through a similar posterior spinal approach as fusion surgery, but only three screws and a single rod are used. Up to 40% of normal spine motion is preserved," says Dr. Milbrandt. "Given our success with VBT, our team was eager to have a device to treat older patients who wished to avoid fusion."
"Children and families should be provided the opportunity to consider all available scoliosis treatment options and be empowered to select the treatment pathway, either fusion or nonfusion, which best matches their interests and values," says Dr. Larson. Although long-term outcomes are forthcoming, preliminary results show that VBT preserves more normal spine motion than fusion surgery.
Mayo Clinic collaborates closely with industry leaders, the Food and Drug Administration, and surgeon research groups, including Setting Scoliosis Straight Foundation, Pediatric Spine Foundation and other patient advocacy groups, to safely introduce new technology and to improve care for children with scoliosis.
Complex spine surgeries
Mayo Clinic pediatric spine surgeons frequently treat patients with severe and complex spinal deformities who require a team-based approach. "Because Mayo cares for patients of all ages, we can draw upon our adult spine, radiology and neurosurgical colleagues for their expertise. Mayo surgeons frequently operate together, because we believe that for complex spinal deformity, the properly assembled team is more robust than any one surgeon alone," says Dr. Larson.
Mayo Clinic offers in-house neurological monitoring services during all spine surgeries, which is specifically helpful for children who may have underlying myelopathy or spinal cord damage prior to surgery. Mayo's cardiac and pediatric postoperative ICU care, cardiac anesthesia, and world-class medical expertise optimize perioperative care for patients with even the most complex medical problems.
Mayo radiologists work with the latest imaging technology and are adept at advanced techniques, including reformatting 3D images from the biplanar X-ray images and printing 3D models based on CT and MRI, to help surgeons individualize the surgical plan for each patient. For complex spine cases, 3D spinal models are printed to scale in-house at Mayo and aid in preoperative planning for the team to confirm appropriate implants and surgical approach.
Intraoperative low-dose CT imaging and computerized navigation may be used during the operation, to ensure accurate placement of implants and appropriate deformity correction. "For a complex deformity case, we may have six to eight face-to-face meetings preoperatively with our multidisciplinary team to develop a plan, optimize the child's medical status, and rehearse the surgery. Our institutional culture of collaboration, teamwork and dedication to patient care leads to superior surgical results," says Dr. Larson.
Routinely, spine imaging at Mayo is performed using low-dose biplanar X-ray, which results in approximately one-fiftieth the dose of a standard office X-ray and also allows better accuracy and image quality. "We take extra care to minimize radiation exposure to children at all visits," says Dr. Larson.
Mayo also specializes in nonoperative scoliosis care. "Our partners in orthotics fabricate custom braces, including thoracic lumbar sacral orthosis braces, Boston-type braces and Rigo Cheneau braces. Our pediatric orthopedic team works with Mayo Clinic therapists trained in scoliosis-specific exercises, or the Schroth method, to build muscle strength to slow curve progression. We have a high success rate in treating scoliosis without surgery, either using customized braces or, for severe scoliosis in children typically under age 3, placement of a Mehta or body cast," says Dr. Larson.
Early-onset scoliosis can also be treated with magnetically controlled growing rods or other approaches to preserve spinal growth, such as VBT.
Multimodal pain control
For any child receiving surgical treatment at Mayo Clinic, pain control is of the utmost importance to ensure a safe and comfortable recovery. Because Mayo Clinic routinely offers pediatric spine surgery, experienced teams including surgeons, child life specialists, pediatric nurses, physical therapists and anesthesiologists work together to provide superior pain control.
A patient's postoperative pain management plan may include intraoperative spinal injections, visits from child life specialists, early walking, local anesthetic injected into the surgical wound, and sometimes indwelling pain catheters. Most patients do not require postoperative IV narcotics and are transitioned quickly to a regular diet and oral pain medications. "Patients eat and walk the day after surgery, and these measures have reduced length of stay in the hospital to two to three days," says Dr. Milbrandt. "In summary, Mayo surgeons continue to safely innovate to bring the best strategies in spine care to pediatric patients."
For more information
Mayo Clinic Children's Center. Mayo Clinic.
The Tether — Vertebral Body Tethering System — H190005. U.S. Food and Drug Administration.
Minimally Invasive Deformity Correction (MID-C) System — H170001. U.S. Food and Drug Administration.