Sept. 30, 2022
In a prospective, self-controlled clinical trial published in Investigative and Clinical Urology in March 2022, Mayo Clinic investigators found that both pessary use and surgery for pelvic organ prolapse improved symptoms. However, patients deemed the degree of improvement more significant for surgery.
Unique study design
This study's novelty, according to senior study author John A. Occhino, M.D., M.S., Female Pelvic Medicine and Reconstructive Surgery at Mayo Clinic's Minnesota campus, lies in the study design: each participant comparing experience with one modality to that with the other. Each study participant served as the control to conduct a direct comparison between pessary and surgery. Findings with this study design can be valid despite smaller participant numbers compared with other designs, and the design also improved the quality of the study's findings, says study first author Brian J. Linder, M.D., Female Pelvic Medicine and Reconstructive Surgery at Mayo Clinic's Minnesota campus.
All patient intervention needs derived from self-identified prolapse symptom bother, which Dr. Occhino indicates can make therapeutic objectives "super gray." Study participants elected surgery after their physicians explained the therapeutic options: observation, pessary or surgery. Following this decision, their physicians invited them to participate in the study. Rather than randomizing participants to pessary use or surgery — challenging since most women want to choose their interventions personally, per Dr. Linder — the physicians asked each participant to undergo the same two therapies. The study required surgery be scheduled between seven and 30 days after consult, with a pessary worn pre-surgically.
الرفو المهبلي وتثبيت المهبل العَجُزي
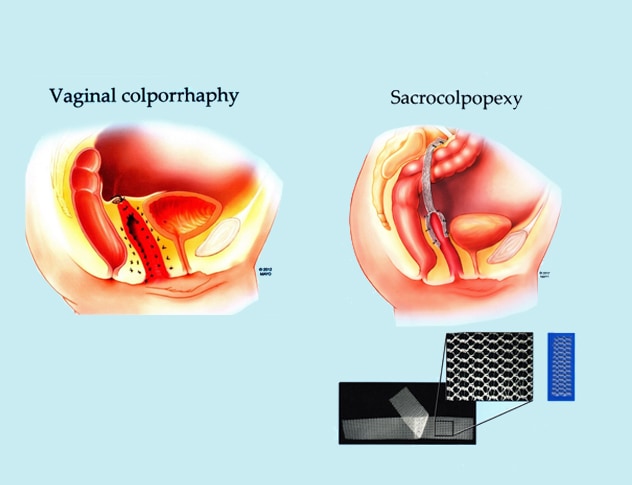
الرفو المهبلي وتثبيت المهبل العَجُزي
يُستخدم إجراء الرفو المهبلي (جراحة عبر المهبل) وتثبيت المهبل العَجُزي لجراحة تدلي أعضاء الحوض.
The investigators used the Patient Global Index of Improvement to measure prolapse symptom effects on patients' day-to-day lives at baseline, after pessary use and three months post-surgically for those completing surgery, allowing recovery time and return to regular activity. Of 61 participants, 40 underwent both treatments and directly compared pessary use and surgery with 33 preferring surgical outcomes, five indicating the same outcomes with each therapy and two indicating greater symptom improvement with a pessary. Improvements measured included pressure, bulge and heaviness based on the validated questionnaire.
Points to note about the study
Drs. Occhino and Linder indicate notable items in this study:
- Due to the geographical location of the study — Upper Midwest — participants were mostly white.
- All patients decided on surgery before study enrollment.
- Of the study participants,19% decided against surgery, electing to continue with pessary use after trialing the device and determining that it sufficiently controlled their symptoms.
- The investigators based participants' outcomes at three months post-surgery on a survey rather than on physical exam.
The reason for surgical treatment outcome preference is currently unknown and needs further research, says Dr. Occhino.
"We don't know why surgery had better improvement, says Dr. Linder. "Perhaps surgery had better anatomical correction or the pessary contributed to a degree of pelvic pressure in some."
Dr. Linder notes that future research could measure anatomical correction via imaging with a pessary and post-surgically.
"What I'd say to a patient bothered by prolapse symptoms is that we've seen patients improve with a pessary or surgery," Dr. Occhino says. "The pessary's benefit is it's nonsurgical and no risk; the negative is also that it's nonsurgical — or not permanent."
Dr. Linder echoes these sentiments. "There's no wrong answer — at the end of the day patients get to choose what treatment sounds right for them," he says. "Most patients are eligible for multiple options. If patients achieve their treatment goals and symptoms improve, that is what we are looking for, whether it's surgical or not."
Pelvic organ prolapse therapeutic goals
A current pelvic organ prolapse therapy trend is subjective surgical outcome assessment versus solely anatomical assessment, says Dr. Occhino. Ideally, Dr. Linder says, improvement includes symptomatic relief and anatomical correction.
In purely anatomical assessment, Dr. Occhino explains the female pelvic medicine and reconstructive surgery field considers any small return of prolapse an interventional failure, even if the patient is unaware of this and feels satisfied. This is complicated by variations in patients' distinct prolapse experiences, with differing symptom combinations and tolerances.
"Satisfaction with a pessary is super personal," says Dr. Occhino. "Almost one-fifth of our study participants liked them enough that they wanted to cancel surgery. Some didn't like the pessary or said it helped but that a pessary was not for them. Other participants made comments such as 'Oh my gosh, I'm so thankful I don't have to have surgery'; but some said, 'Heard about it; don't want it.' "
While providers have previously used a pessary as a diagnostic trial — using information gleaned to determine potential surgical benefit — Dr. Linder indicates that this has been an empirical practice.
"This study supports providers in this practice somewhat, as patients typically do as least as well with surgery as with a pessary," says Dr. Linder. "It demonstrates that one of a pessary's roles is demonstrating for patients the potential improvement with surgery."
Reasonable prolapse intervention goals include no vaginal area pressure and bulge. If the patient has overactive bladder, however, prolapse surgery may improve symptoms or patients may require distinct therapy.
"Urinary symptoms may or may not be related to pelvic organ prolapse," Dr. Occhino says. "I tell a patient with prolapse surgery the bulge will be gone; I don't know how it will affect the overactive bladder."
Pain relief is an atypical prolapse therapeutic goal, he says, as the condition is not typically painful.
"If a patient's experiencing pain, there's probably something else going on," indicates Dr. Occhino.
Pelvic organ prolapse referral benefits
Dr. Occhino believes that community surgeons with solid prolapse surgery skill sets and training can treat patients locally. If not, he indicates sending patients to a female pelvic medicine and reconstructive surgery (FPMRS)-certified surgeon may be wise.
He suggests considering referral not only due to a certified surgeon's volumes and experience with prolapse but also because a specialty clinic can offer an environment specifically designed for treating prolapse.
For instance, Dr. Occhino says stocking thousands of pessaries to fit different anatomies can be unrealistic for community surgeons, so many stock only the commonly used ring pessaries.
A common patient complaint with pessaries is falling out, he says. A specialty center such as Mayo Clinic, however, has multiple other pessary options that may better fit the anatomy.
"If you wore tennis shoes and they gave you a blister, you wouldn't say you could never wear tennis shoes again," he says. "They're probably just the wrong size; you need another option."
Dr. Occhino explains that in a specialty female pelvic medicine and reconstructive surgery (FPMRS) clinic, physicians also have more time to offer patients.
"You can't successfully assess urinary function, sexual function and other functions in a 15-minute visit," he says. "We have time in our clinic to assess all these issues and look at the gamut of treatment options. A full assessment is most useful to patients with prolapse symptoms."
Mayo Clinic's specialty FPMRS clinic also offers one-day patient visits for prolapse, including all testing and physician appointments, making the process easy and efficient for nonlocal patients.
Although physician referral to Mayo Clinic's FPMRS clinic is useful with its accompanying medical documentation and is helpful for subspecialist relationship building, patients may self-refer as well.
"What should drive patients and their physicians to seek evaluation is bothersome symptoms," says Dr. Occhino, citing an "if it ain't broke, don't fix it" approach in the field.
For more information
Linder BJ, et al. Comparison of outcomes between pessary use and surgery for symptomatic pelvic organ prolapse: A prospective self-controlled study. Investigative and Clinical Urology. 2022;63:214.
Refer a patient to Mayo Clinic.