March 26, 2022
A Mayo Clinic study suggests that the pathogenesis of stroke in individuals with coronavirus disease 2019 (COVID-19) is an interplay of vascular risk factors and immune responses to the SARS-CoV-2 virus.
Immune responses to the virus have generally been thought to play a role in the significantly increased risk of stroke for individuals with COVID-19. However, data on the role of traditional vascular risk factors have been mixed.
نموذج تخطيطي لأسباب نشوء المرض المقترحة
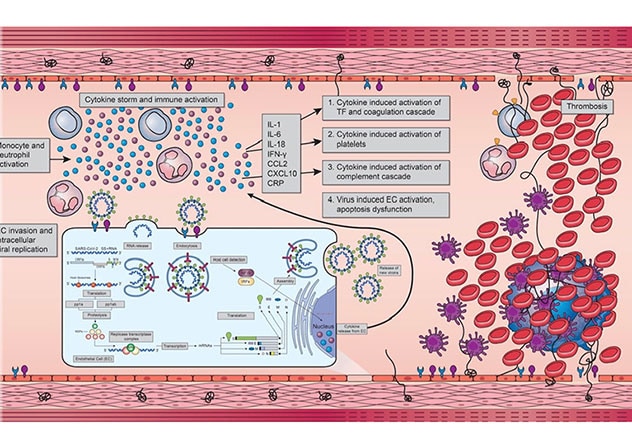
نموذج تخطيطي لأسباب نشوء المرض المقترحة
يرتبط فيروس سارس كوف-2 بالخلايا البطانية الوعائية. وتُطلق الخلايا المصابة كيموكينات وسيتوكينات، والتي تتسبب في إصابة الخلايا الوحيدة والبلعمية. وتنتج هذه الخلايا مزيدًا من السيتوكينات الالتهابية، الأمر الذي يؤدي في النهاية إلى حدوث عاصفة السيتوكين. وتنشط الصفائح الدموية، وكذلك عوامل تخثر الدم. والمرضى المصابون بعوامل خطر متعلقة بالأوعية الدموية، مثل داء السكري وفرط ضغط الدم وارتفاع دهون الدم والسمنة، يكون لديهم بالفعل إصابة في الخلايا البطانية الوعائية مع خطورة إصابة الأوعية الدموية.
"We found that the interplay between the preexisting vascular risk factors and the immune response in COVID-19 results in an amplified, robust, inflammatory reaction, and contributes to vessel thrombosis, occlusion and ultimately stroke," says Bart M. Demaerschalk, M.D., a stroke neurologist at Mayo Clinic in Phoenix/Scottsdale, Arizona, and senior author of the study.
As described in Mayo Clinic Proceedings: Innovations, Quality & Outcomes in 2022, the study retrospectively evaluated individuals who had both COVID-19 and stroke diagnoses within a three-month period. Most case series have described the acute stroke characteristics in patients with simultaneous COVID-19.
The Mayo Clinic study evaluated the records of patients nationwide who were hospitalized at Mayo Clinic and who had diagnoses of stroke and COVID-19 infection within a three-month interval between September 2019 and December 2020. Only adults with a confirmed new diagnosis of acute ischemic or hemorrhagic stroke and a confirmed COVID-19 diagnosis were included. Thirty individuals met the study criteria.
Key findings include:
- A low stroke rate — just 0.5% — among Mayo Clinic patients hospitalized with COVID-19
- A high proportion of individuals — more than 80% — with at least one traditional stroke risk factor, such as hypertension, hyperlipidemia, smoking history, diabetes or atrial fibrillation
- Elevated serum biomarkers for inflammation and coagulation in individuals for whom those laboratory values were available
- A low rate — only 7% — of individuals with acute ischemic stroke who were treated with intravenous alteplase
- A mortality rate of 37% among the individuals studied
"The low rate of reperfusion therapy was mostly due to late presentation at the hospital — likely because individuals were hesitant to go to the hospital in the midst of the pandemic," Dr. Demaerschalk says. "Significant efforts are needed to combat hesitancy toward hospital presentation to improve the number of patients eligible for acute stroke therapy." Early recognition remains critical when serious COVID-19 infection complicates an acute ischemic stroke.
"Treatment includes simultaneously combating the COVID-19 infection with antiviral, anti-inflammatory medications and supportive care, whilst attempting to recanalize occluded arteries with pharmacological and mechanical means," Dr. Demaerschalk says.
For more information
Mbonde AA, et al. Stroke features, risk factors and pathophysiology in SARS-CoV-2 infected patients. Mayo Clinic Proceedings: Innovations, Quality & Outcomes. In press.
Refer a patient to Mayo Clinic.