March 20, 2021
Specialists at Mayo Clinic Children's Center in Rochester, Minnesota, can provide innovative treatments for children with epilepsy. Working closely with Mayo Clinic research teams, these specialists are able to offer cutting-edge options to eliminate or reduce seizures in children.
"Experts from various specialties come together to make decisions about medications and treatments. The research and clinical teams function seamlessly together," says Kai J. Miller, M.D., Ph.D., a neurosurgeon at Mayo Clinic Children's Center. "We're actively developing new technology so patients can receive the most novel therapies to treat seizures and preserve brain function."
Mayo Clinic Children's Center has a pediatric team dedicated to the care of children with epilepsy. All children undergo MRI using specialized protocols developed by Mayo Clinic's neuroradiology epilepsy experts. Some of these patients might be eligible for enrollment in clinical trials. In addition to offering medical treatments, the Mayo team can provide holistic care for the child and family, addressing the learning and behavioral challenges that often are seen.
After an initial evaluation, children and their parents can choose from a number of available options to reduce seizure frequency and severity. "For some children with drug-resistant epilepsy, surgery is an option. But for others, a unique type of medication or diet therapy can decrease seizure frequency and severity," says Elaine C. Wirrell, M.D., a pediatric epileptologist at Mayo Clinic Children's Center and co-founder of the Pediatric Epilepsy Research Consortium.
Surgical options
As a level 4 comprehensive epilepsy center, the highest rating designated by the National Association of Epilepsy Centers, Mayo Clinic uses advanced surgical techniques, including robotic guidance during resective surgery. "With that guidance, surgeons can more precisely identify where seizures start — which allows us to target the seizures and stop them," Dr. Miller says.
Laser interstitial thermal therapy may be an option for some children. In this less invasive technique, MRI is used to guide the surgeon to place a probe through a small hole in the skull. A laser pinpoints and destroys a small portion of brain tissue. "This therapy actually burns and destroys the place in the brain where the seizure originates, and does so without injuring the rest of the brain or requiring a large surgery," Dr. Miller says. Other surgical options include:
Corpus callosotomy
Used to treat children who experience frequent drop seizures leading to repeated and abrupt falls, corpus callosotomy severs the bundle of nerves connecting the right and left sides of the brain. Drop seizures are eliminated or markedly decreased for most children, preventing ongoing injury.
Hemispherotomy
Children who experience seizures that originate from multiple sites in one hemisphere often require this surgery. It disconnects the abnormal, seizure-inducing hemisphere, allowing the other hemisphere to function normally and stopping the seizures.
For children who have severe epilepsy or who cannot have surgery, neurostimulation treatments might be an option. These therapies apply electricity to the central nervous system with the goal of reducing seizure frequency and severity. Some neurostimulation treatments require surgical implantation of a device.
In a review published in the October 2019 issue of Brain Sciences, Mayo Clinic researchers found that neurostimulation is safe and effective and proposed a methodology for selecting among available options for children with epilepsy. Those options include:
Vagus nerve stimulation
This treatment sends regular, mild pulses of electrical energy to the brain via the vagus nerve in order to prevent seizures. A stimulator device is implanted under the skin in the chest, and a wire is wound around the vagus nerve in the neck.
Responsive neurostimulation
This type of neurostimulation monitors brain waves and responds to electrical activity that looks like a seizure. This stops seizures before they cause clinical symptoms.
Deep brain stimulation
Mayo Clinic is one of the leading sites in the United States for this therapy, which delivers controlled pulses to a target in the brain that is part of a circuit involved in seizures.
الكبت المستمر للنوبات
الكبت المستمر للنوبات
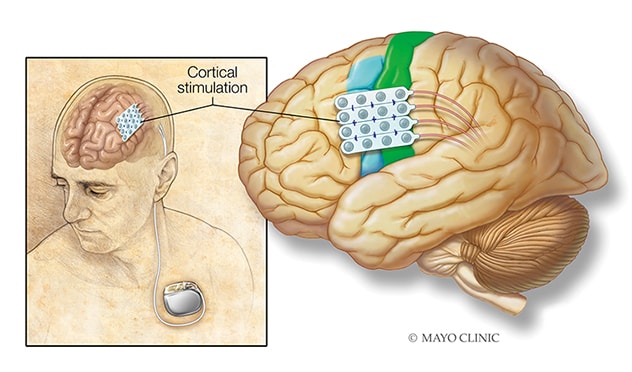
يستخدم التنبيه القشري المزمن تحت العتبة، أقطاب كهربائية تُزرَع جراحيًّا في مكان ظهور النوبة، وتتصل هذه الأقطاب الكهربائية بمولِّد مزروع في الصدر.
التحفيز غير المتوغل للدماغ
التحفيز غير المتوغل للدماغ
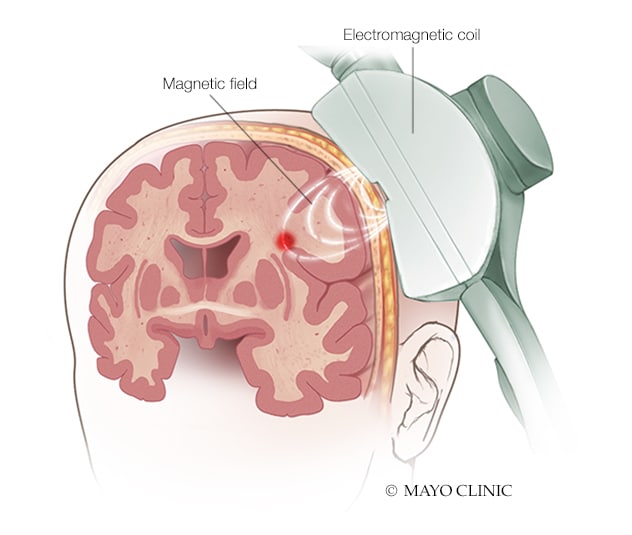
في التحفيز المغناطيسي عبر الجمجمة، يولّد ملف كهرومغناطيسي يوضع أمام فروة الرأس مجالاً مغناطيسيًّا يعمل بدوره على تحفيز مناطق معينة في الدماغ.
Chronic subthreshold cortical stimulation
In some children, a responsive device might not detect abnormal electrical activity in time to prevent a seizure. Subthreshold cortical stimulation provides continuous electrical impulses to an area of seizure onset to suppress the generation of the abnormal seizure discharge and thus attenuate the seizure.
Transcranial magnetic stimulation
An electromagnetic coil placed against the scalp delivers a magnetic pulse that stimulates nerve cells in the brain.
Transcranial direct current stimulation
This technique applies a low-intensity current that manipulates neuronal activity and neuroplasticity.
Rare epilepsy syndromes
Mayo Clinic is researching innovative medications and participating in clinical trials for the treatment of rare but severe epilepsy syndromes, including Dravet syndrome and Lennox-Gastaut syndrome, as well as epilepsy syndromes with rare causes, such as CDKL5 deficiency disorder.
"As neurologists, we provide precision therapies through advanced understanding of etiologies and preferred treatments, such as potassium channel blockers for patients with potassium channel-related epilepsy encephalopathies and fenfluramine, stiripentol and cannabidiol for patients with Dravet syndrome," says Katherine C. Nickels, M.D., a pediatric epileptologist at Mayo Clinic Children's Center in Rochester, Minnesota. "While many therapies such as stiripentol are considered to be new in most institutions, they are the standard of care at Mayo Clinic."
Studies and trials that Mayo Clinic has led or participated in include:
- A clinical trial of a gene therapy known as STK-001 for the treatment of Dravet syndrome. "This therapy has the potential to prevent not only seizures but also the neurocognitive regression that these children have," Dr. Wirrell says.
- A clinical trial of the neurosteroid ganaxolone for children and young adults with CDKL5 deficiency disorder.
- Three clinical trials investigating the efficacy of cannabidiol therapy in children with Dravet syndrome, Lennox-Gastaut syndrome and tuberous sclerosis complex. "All of those trials found that cannabidiol provided greater benefits than placebo," Dr. Wirrell says.
- A study published in the January 2021 issue of Epilepsia that found that the ketogenic diet was the most effective treatment studied for children with myoclonic atonic epilepsy.
"For many children with early-onset epilepsy, the prognosis using conventional therapies has been quite poor," Dr. Wirrell says. "We feel it's important to continue participating in clinical trials and other studies, as a precision medicine approach allows our patients to receive the best possible therapies."
For more information
Pediatric Epilepsy Research Consortium.
National Association of Epilepsy Centers.
Starnes K, et al. A review of neurostimulation for epilepsy in pediatrics. Brain Sciences. 2019;9:283.
Stoke Therapeutics, Inc. An Open-Label Study To Investigate the Safety and Pharmacokinetics of Single Ascending Doses of Antisene Oligonucleotide STK-001 in Children and Adolescents With Dravet Syndrome. ClinicalTrials.gov.
Marinus Pharmaceuticals. Study of Adjunctive Ganaxolone Treatment in Children and Young Adults With CDKL5 Deficiency Disorder (Marigold). ClinicalTrials.gov.
Nickels K, et al. Epilepsy with myoclonic-atonic seizures (Doose syndrome): Clarification of diagnosis and treatment options through a large retrospective multicenter cohort. Epilepsia. 2021;62:120.
Refer a patient to Mayo Clinic.