Oct. 01, 2022
Mayo Clinic Children's Center has the expertise needed to develop optimal treatment plans for children with brain tumors. Specialists in the Pediatric Brain Tumor Clinic can often see patients within a day of referral.
"Our multidisciplinary team can be put into place very quickly," says Jonathan D. Schwartz, D.O., M.P.H., a pediatric neuro-oncologist at the Mayo Clinic Children's Center in Rochester, Minnesota. "We communicate with one another so everyone is on the same page, and families can quickly get a detailed diagnosis and a treatment plan."
The specialized treatment required for pediatric brain tumors differs from the regimens used in adults. The Pediatric Brain Tumor Clinic focuses on the specific needs of children while drawing on the broad resources of a major tertiary center.
The care team includes specialists in pediatric neurology, pediatric neurosurgery, neuroradiology, pediatric endocrinology, neuropathology, pediatric radiation oncology, pediatric oncology, child psychology and pediatric rehabilitation. For complex tumor resections, pediatric neurosurgeons often collaborate with colleagues in adult neurosurgery, otolaryngology/head and neck surgery and neuro-ophthalmology.
"We might work, for example, with skull base or peripheral nerve surgeons who are recognized as leaders in their field," says David J. Daniels, M.D., Ph.D., a pediatric neurosurgeon at Mayo Clinic's campus in Minnesota. "This collaboration allows us to manage cases that can't be easily done elsewhere."
Routine multidisciplinary collaboration
As a designated comprehensive cancer center, Mayo Clinic meets the National Cancer Institute's strict standards for scientific excellence and a multispecialty approach focused on cancer prevention, diagnosis and treatment.
Specialists in the Pediatric Brain Tumor Clinic work together to treat children with various types of disease, including:
- Medulloblastoma
- Embryonal tumor
- Glioma, including astrocytomas, ependymomas and oligodendrogliomas
- Germ cell brain tumor
- Infant brain tumor
- Spinal cord tumor
- Craniopharyngioma
A multidisciplinary pediatric brain tumor board meets weekly to recommend optimal approaches to individuals' diseases.
"We discuss our own patients' cases, as well as outside cases, to determine if there is an approach that might help," says Nadia N. Laack, M.D., chair of Radiation Oncology in the Children's Center at Mayo Clinic's campus in Minnesota. "Our model of care ensures that each patient has a thorough case review, and potentially access to new radiation techniques or surgical options."
الورم البطاني العصبي مرتفع الدرجة
الورم البطاني العصبي مرتفع الدرجة
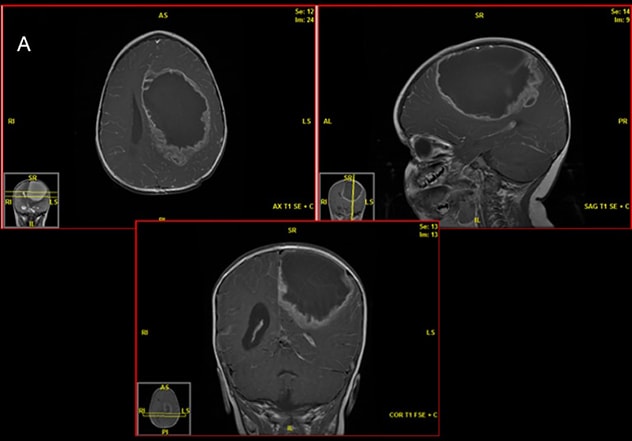
يُظهر التصوير بالرنين المغناطيسي الذي أُجري قبل الجراحة ورمًا بطانيًا عصبيًا مرتفع الدرجة لدى مريض يبلغ من العمر 18 شهرًا.
دليل علم أمراض الأنسجة
دليل علم أمراض الأنسجة
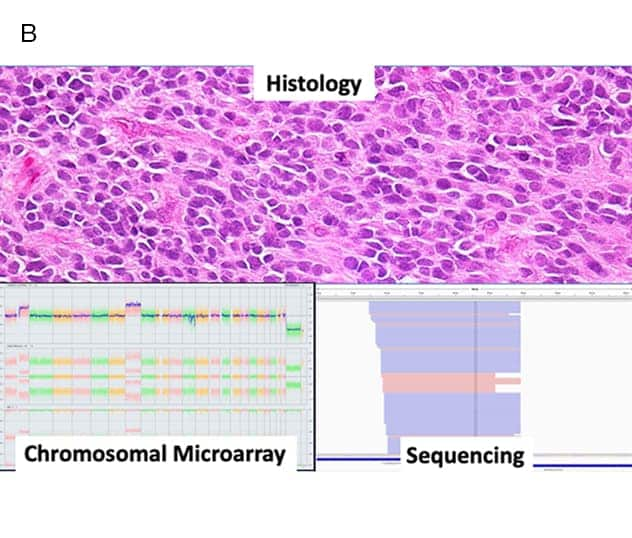
يُظهر فحص أمراض الأنسجة ورمًا كشميًا بطانيًا عصبيًا مع تسلسل لاحق ومصفوفات صبغية دقيقة توضح اندماج RELA، ويؤكد على أنه من الأفضل الخضوع للعلاج الإشعاعي.
العلاج بالإشعاع البروتوني
العلاج بالإشعاع البروتوني
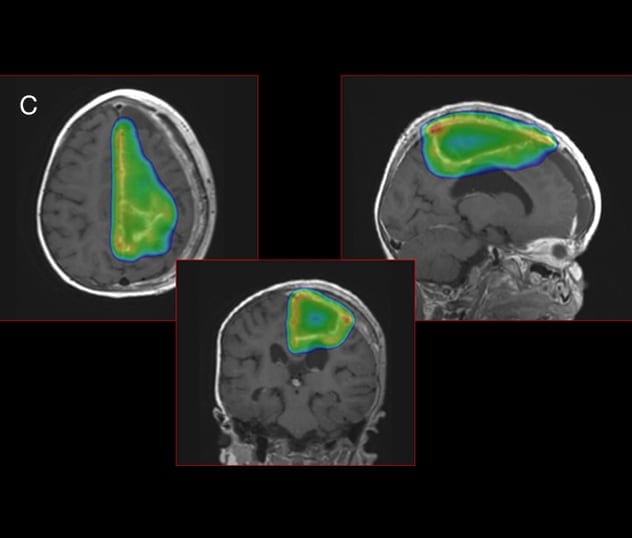
لتجنب التسمم في أنسجة المخ المحيطة، تلجأ مايو كلينك لاستخدام العلاج بالإشعاع البروتوني. تُظهر سحابة جرعة البروتون، الموضحة بالألوان، التوافق الوثيق للعلاج بالبروتون مع ورم الطفل.
The tumor board also incorporates Mayo's expertise in neuropathology. Genetic mutations in pediatric brain tumors can differ from the mutations seen in similar tumors in adults. The integration of comprehensive genetic testing, such as neuro-oncology-specific next generation sequencing and chromosomal microarray analysis, can provide more-detailed information about an individual child's brain tumor.
"That's especially helpful for tailoring therapy directly to the patient if a tumor has a risk of recurrence," says Gesina F. Keating, M.D., a pediatric neuro-oncologist at Mayo Clinic's campus in Minnesota.
Cutting-edge technology
State-of-the-art imaging is a key component of Pediatric Brain Tumor Clinic care. Subspecialized neuroradiologists use:
- 7-tesla MRI, for greater clarity compared with conventional 3-tesla MRI
- Magnetic resonance elastography to assess a tumor's firmness
- Slip interface imaging to reveal the extent of tumor adhesion
- 3D-printed models of patients' brains and tumors to guide surgical planning
Mayo Clinic is also one of a limited number of centers in the United States that offer proton beam therapy for select children with brain tumors. Mayo Clinic uses the latest form of this therapy to closely target the tumor while sparing healthy tissue.
"Children who get proton treatment have fewer side effects in terms of IQ changes, cognitive development, growth, and endocrine development and hormonal problems than children who have traditional radiotherapy," Dr. Laack says.
That reduced toxicity can be achieved without compromising tumor outcomes. As described in the Sept. 1, 2019, issue of the International Journal of Radiation Oncology, Biology, Physics, the two-year survival rate for children with brain tumors treated with pencil beam scanning therapy at Mayo Clinic is 93%.
Gamma Knife radiosurgery is used in selected pediatric patients with benign brain tumors as well as metastatic disease. Medications that target unique mutations in pediatric tumors also may be used. These targeted drug therapies can offer more precision than broader acting chemotherapy drugs.
Laser ablation is another option. Mayo Clinic is one of the few centers that offer this minimally invasive procedure to treat certain types of pediatric brain tumors, avoiding the need for craniotomy.
"We use laser ablation for small, spherical tumors," Dr. Daniels says. "We can make a small burr hole, insert a laser, get a biopsy and then ablate with MRI guidance." Although data on long-term outcomes aren't yet available, Dr. Daniels notes that short-term outcomes are promising.
Pediatric brain tumors pose unique challenges and require highly specialized expertise. "The entire resources of Mayo Clinic's strong neuro-oncology program are available to our pediatric patients," Dr. Laack says.
For more information
Pediatric Brain Tumor Clinic. Mayo Clinic.
Rongthong W, et al. Effect of prospective use of radiobiologic effect (RBE) modeling in treatment planning on magnetic resonance imaging (MRI) radiation related changes (RRC) in pediatric patients with brain tumors treated with pencil beam scanning proton therapy (PBS). International Journal of Radiation Oncology, Biology, Physics. 2019;105:E628.
Refer a patient to Mayo Clinic.