April 13, 2019
The impact of the obesity epidemic on the incidence of liver disease is increasing. Obesity is a key risk factor in the development of nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH). Both of these conditions are significant risk factors for liver failure and can lead to the need for liver transplantation (LT). Patients with other chronic liver diseases frequently struggle with obesity as well. Excessive weight gain, metabolic syndrome and obesity frequently complicate the post-liver transplant setting.
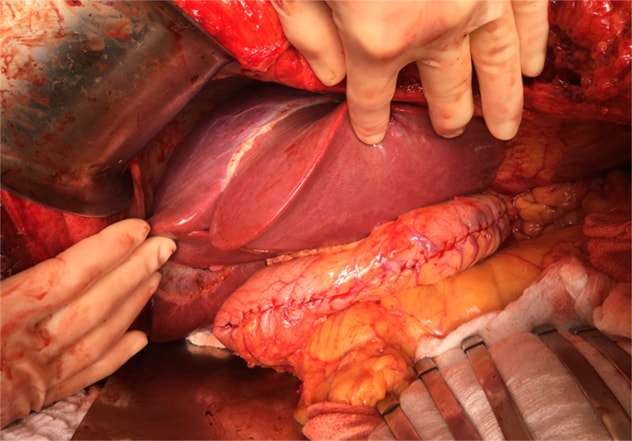
To address this issue, a team of Mayo Clinic researchers recently performed a study comparing patient outcomes associated with two different approaches to weight-loss intervention — lifestyle modification before LT and simultaneous LT plus sleeve gastrectomy (LT plus SG). Mayo researchers shared their study findings in an article published in Hepatology.
According to Kymberly D. Watt, M.D., this study addresses an important challenge encountered in liver transplantation. Dr. Watt is a gastroenterologist and liver transplant specialist at Mayo Clinic's campus in Rochester, Minnesota, and a co-author for the article published in Hepatology.
"We know that obese patients have difficulty accessing transplant services," explains Dr. Watt. "They are less likely to be placed on the waitlist, less likely to undergo transplantation once on the waitlist, and they exhibit higher waitlist mortality. We also know that weight reduction is difficult to achieve and sustain, especially for people with long-standing, severe medically complicated obesity."
Mayo researchers note that obesity before transplant and weight gain after transplant are also associated with major risk factors for post-transplant cardiovascular events and the onset or recurrence of NASH.
Study methods
A multidisciplinary team led by transplant surgeon Julie K. Heimbach, M.D., enrolled study participants with a body mass index (BMI) ≥ 35 kg/m2 referred for LT since 2006. All study participants were enrolled in an aggressive lifestyle modification weight management protocol before transplant surgery. Dr. Heimbach is chair of Transplantation Surgery at Mayo Clinic's campus in Rochester, Minnesota, and senior author for the Hepatology article.
Study participants were divided into two cohorts. The "LT alone" cohort included participants who underwent LT after achieving the weight-loss target (BMI < 35) and a Model for End-Stage Liver Disease (MELD) score high enough to access transplantation.
 الزراعة المتزامنة للكبد مع تكميم المعدة
الزراعة المتزامنة للكبد مع تكميم المعدة
يعد الجمع بين زراعة الكبد وتكميم المعدة طريقة معالجة تهتم بعلاج أمراض الكبد، وتؤدي إلى فقدانٍ معقول للوزن.
The "LT plus SG" cohort included participants who had a MELD score high enough to access transplantation but who did not achieve a BMI target of < 35 before surgery. This cohort underwent simultaneous LT plus SG.
Study findings
The study summarized outcomes for all patients who have undergone combined LT plus SG to date (n = 27). Focusing on those with three or more years of follow-up (n = 17), the researchers' goal was to determine the long-term impact of combined LT plus SG compared with LT alone. Significant findings include the following:
- In the LT alone cohort, 83.3 percent (30 of 36 participants) achieved > 10 percent loss in total body weight (TBW) before LT.
- Three years after transplant, 29.4 percent of participants in the LT alone cohort maintained > 10 percent loss in TBW vs. 100 percent of the participants in the LT plus SG cohort (P < 0.001).
- Participants in the LT plus SG cohort maintained a significantly higher percentage of total body weight loss after three years of follow-up (LT alone cohort, 3.9 ± 13.3 percent vs. LT plus SG cohort, 34.8 ± 17.3 percent (P < 0.001).
- Participants in the LT plus SG cohort had a lower prevalence of hypertension, metabolic syndrome, insulin resistance and hepatic steatosis. This cohort also required fewer antihypertensive medications and lipid agents at last follow-up than did the LT alone cohort.
Conclusions
Although weight loss before transplantation was achieved by obese patients in both cohorts, participants in the LT plus SG cohort had a more effective and durable weight loss than did participants in the LT alone cohort. The LT plus SG participants also had fewer metabolic complications at last follow-up.
"Because obesity-related liver disease is now one of the most common indications for liver transplantation, identifying a structured approach to manage or prevent excessive weight gain before and after transplantation is an important goal," says Dr. Watt.
Mayo researchers note that more research is needed to define the optimal timing and selection criteria for the combined LT plus SG procedure. "Combined LT plus SG is an approach that cures liver disease and provides durable weight loss, restoring patients to full function," says Dr. Heimbach. "However, whether the optimal timing is a combined approach or a staged approach — with LT followed by SG at four to 12 months — remains a question for further study. Another key question is addressing weight gain in those patients who underwent LT alone, and whether some should be selected for either a combined LT plus SG or an early post-LT SG."
For more information
Zamora-Valdes D, et al. Long-term outcomes of patients undergoing simultaneous liver transplantation and sleeve gastrectomy. Hepatology. 2018;68:485.