Oct. 23, 2018
Worldwide, esophageal cancer is the eighth most common cancer, the sixth most common cause of cancer-related deaths, and the most rapidly rising cancer in developed countries. The two most common forms of esophageal cancer are esophageal squamous cell carcinoma (ESCC) and esophageal adenocarcinoma (EAC).
Incidence and risk factors
ESCC is the most prevalent form of esophageal cancer worldwide, but its incidence varies among geographic regions. The highest rates of ESCC are found in less developed countries and regions, including north-central China, Iran, central Asia, and eastern and southern Africa.
Epidemiologic associations for ESCC also vary. In high-risk regions, major risk factors include exposure to carcinogens, poor oral hygiene, opium use, poor nutrition and thermal damages caused by hot beverages. In low-risk regions, including the United States and other developed countries, tobacco exposure and alcohol consumption are the most strongly linked risk factors. Dysplasia is the precursor lesion that can progress to ESCC.
EAC is the most prevalent form of esophageal cancer in the United States and other developed countries in the Western Hemisphere. Barrett's esophagus (BE) is the main precursor to EAC. This condition is marked by a change in the esophageal epithelium of any length and is due to chronic gastroesophageal reflux disease (GERD). Other risk factors include obesity, smoking, male sex and Caucasian race.
The incidence of EAC in Europe and North America is increasing rapidly. EAC is more common among white men, those with a history of chronic GERD and central obesity, and a family history of BE and EAC.
Screening strategies and challenges
One of the challenges associated with both EAC and ESCC is the fact that most patients who have esophageal cancer seek medical care only when they have trouble swallowing, when the cancer is advanced and the potential for survival is very limited. The five-year survival rates are substantially better for people diagnosed with early asymptomatic cancers than for those diagnosed with symptomatic disease. Both EAC and ESCC diagnosed after the onset of symptoms have a five-year survival rate of less than 20 percent.
Early detection is associated with improved survival rates for both ESCC and EAC. However, noninvasive, low-cost screening tools for these cancers are currently not employed. The lack of an accurate, cost-effective and widely accepted screening tool, difficulty in defining a well-characterized screening population, and the absence of data on the costs of noninvasive screening are a few of the issues that remain to be resolved.
ESCC
There are currently no guidelines recommending screening for ESCC in the United States except for individuals with uncommon conditions such as tylosis and untreated achalasia. The search for nonendoscopic screening tools that are reliable, well-tolerated and cost-effective is underway.
كبسولة إسفنجية سليمة وأخرى متوسعة تستخدم في فحص الخلايا الإسفنجي
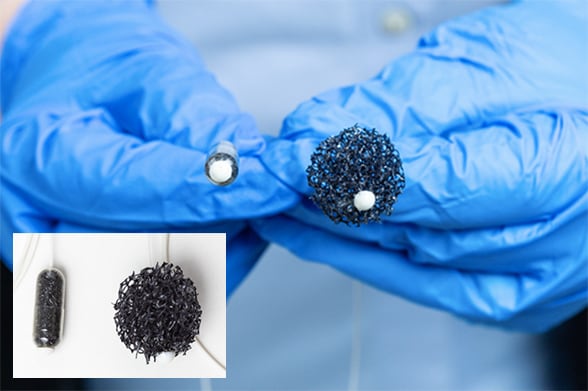
كبسولة إسفنجية سليمة وأخرى متوسعة تستخدم في فحص الخلايا الإسفنجي
قد يكون استخدام فحص الخلايا الإسفنجي والمؤشرات الحيوية من الأدوات الفعالة للكشف المبكر عن سرطانة الخلايا الحرشفية المريئية.
According to David E. Fleischer, M.D., a gastroenterologist at Mayo Clinic's campus in Arizona, "Nonendoscopic screening methods are appealing due to their affordability, ease of use and patient acceptance, but they have some limitations." Balloon cytology is limited by sensitivity and specificity. Sponge cytology has provided some encouraging results related to BE and EAC, but to date, there have been no large studies evaluating this technique for detecting dysplasia related to ESCC. Dr. Fleischer notes that researchers are hopeful that the use of sponge cytology in combination with biomarkers may provide an effective tool for early detection of esophageal dysplasia or ESCC.
المخاط الطبيعي باستخدام التصوير التنظيري بالضوء الأبيض وآفة غير مصبوغة بتلوين لوجول التنظيري
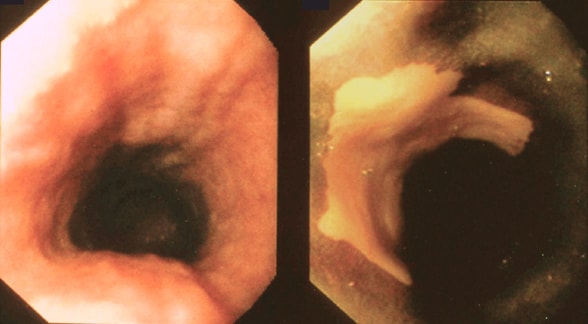
المخاط الطبيعي باستخدام التصوير التنظيري بالضوء الأبيض وآفة غير مصبوغة بتلوين لوجول التنظيري
مخاط طبيعي بالتصوير بالتنظير الداخلي بالضوء الأبيض (يسار) وآفة غير مصبوغة بتلوين لوجول التنظيري (يمين)، يشيران إلى خلل تنسج أو سرطان الخلايا الحرشفية.
Squamous dysplasia is not always visible with routine white light endoscopy. Because staining with Lugol's solution improves the sensitivity of detection, Lugol's chromoendoscopy is helpful in both discovering premalignant lesions and demarcating them.
In high-incidence areas (China, Iran, Japan, eastern Africa) screening is increasingly employed. Dr. Fleischer and other Mayo colleagues have traveled to China, Iran, and eastern and southern Africa. They are working with colleagues in those regions to help design programs that make early diagnosis of these diseases more possible.
"In high-risk populations, screening programs can be implemented to intervene at a stage when a disease is potentially curable," says Dr. Fleischer. In places such as China, where population-based endoscopic screening for ESCC is already underway in high-incidence areas, researchers are looking for ways to optimize the screening strategy. "We still need to determine which age groups to include and define optimal screening methods and intervals, as well as appropriate follow-up methods," explains Dr. Fleischer.
Prasad G. Iyer, M.D., is a gastroenterologist at Mayo Clinic's campus in Minnesota whose research focuses on early detection of esophageal neoplasia. In an effort to develop novel biomarkers that can be combined with minimally invasive devices to enable population-based widespread screening in endemic areas, Dr. Iyer and colleagues have worked with collaborators in the National Cancer Institute to identify and validate novel methylated DNA markers (MDMs) for the identification of ESCC and squamous dysplasia.
In a tissue-based study using specimens from the United States, China and Iran, they have identified MDMs that can distinguish between normal tissue and ESCC tissue with more than 90 percent accuracy. They have also initiated a pilot study in Kenya testing the feasibility of screening for ESCC and squamous dysplasia using a capsule sponge device.
EAC and BE
Improved outcomes associated with diagnosis and treatment before the onset of symptoms, as well as the development of endoscopic techniques that can successfully treat BE-related dysplasia and early carcinoma, have renewed interest in screening for BE. Several medical society guidelines now recommend screening for BE, followed by endoscopic surveillance.
According to Dr. Iyer, several alternatives to sedated endoscopy are now being evaluated for use as screening tools for BE, associated dysplasia and EAC. "Recent reports on the feasibility and safety of novel nonendoscopic and endoscopic techniques and approaches to screen for Barrett's esophagus are encouraging," says Dr. Iyer. Nonendoscopic approaches currently under investigation include cell-sampling devices, and circulating and exhaled molecular markers.
In the SOS 1 trial, Mayo Clinic researchers led by Dr. Iyer identified, validated and demonstrated the accuracy of novel MDMs for the nonendoscopic diagnosis of BE using a capsule sponge-on-a-string (SOS) cell sampling device. Results from that trial have been accepted for publication in a recent issue of the American Journal of Gastroenterology.
In the SOS 2 trial, Dr. Iyer and colleagues demonstrated that a two-marker MDM panel assayed from SOS samples accurately distinguishes BE cases from controls in a safe and well-tolerated manner. Dr. Iyer and colleagues published an abstract including results from the SOS 2 trial in a recent issue of Gastroenterology. "Although this new screening approach appears to offer some promise, larger studies are indicated and ongoing to confirm these findings," says Dr. Iyer.
Research focused on identifying novel noninvasive biomarkers present in blood, saliva and breath is also in the early stages. "These are a very attractive prospect for screening in view of their safety, ease of use in the primary care setting, and because they do not require physicians to perform the test," explains Dr. Iyer.
Novel endoscopic imaging-based techniques currently under study include esophageal capsule endoscopy (ECE) and unsedated transnasal endoscopy (TNE). Suboptimal accuracy and conflicting results obtained using ECE has made this option look less promising. And although TNE has demonstrated some potential as an accurate alternative to standard endoscopy, its use more broadly as a screening tool may be limited by the fact that currently used devices still require dedicated endoscopy suites, specialized equipment and reprocessing facilities.
In summary, the key to better outcomes for patients with EC is earlier diagnosis. All three Mayo sites utilize the most cutting-edge technologies for early diagnosis and offer endoscopic treatment for disease detected in the pre-malignant phase and for early cancer.
For more information
Wallace MB, et al., eds. Squamous neoplasia of the esophagus. In: Gastroenterological Endoscopy. 3rd ed. Stuttgart, Germany: Thieme Publishers; 2018.
Iyer PG, et al. Highly discriminant methylated DNA markers for nonendoscopic detection of Barrett's esophagus. American Journal of Gastroenterology. 2018;113:1156.
Iyer PG, et al. Accurate non-endoscopic detection of Barrett's esophagus in a multicenter cohort: The SOS 2 trial. Gastroenterology. 2018;154(suppl 1):S-175.