Dense breast tissue: What it means to have dense breasts
Dense breast tissue is detected on a mammogram. People with dense breasts sometimes need additional imaging tests.
By Mayo Clinic Staff
If a recent mammogram showed you have dense breast tissue, you may wonder what this means for your health. Healthcare professionals know that dense breast tissue makes breast cancer screening more difficult. It also increases the risk of breast cancer.
Review your breast cancer risk factors with your healthcare team. Together you can consider your options for additional breast cancer screening tests and decide what's best for you.
What does it mean when your breasts are dense?
Dense breast tissue refers to the way breast tissue looks on a mammogram. It's a very common finding. It doesn't mean there's something wrong.
The breasts are made up of dense breast tissue and fatty breast tissue. Dense breast tissue includes the milk glands, milk ducts and supportive tissue in the breast. Fatty tissue is made of fat cells. A person with dense breast tissue has more dense tissue than fatty tissue.
On a mammogram image, the fatty breast tissue is transparent. It's easy to see through to look for anything concerning. The dense breast tissue looks solid white on the mammogram image. It's hard to see through. Breast cancer, which also looks solid white on a mammogram, could be missed.
How do I know if I have dense breast tissue?
The only way to know if you have dense breast tissue is to have a mammogram. A mammogram is an X-ray of the breast tissue.
The healthcare professional who looks at your mammogram images decides whether you have dense breast tissue. This health professional is typically a radiologist. Radiologists are doctors with special training to interpret the images from an exam. The radiologist compares the amount of fatty tissue to dense tissue. Then the radiologist decides the level of breast density. Sometimes a computer program figures out the level of density in the images and the radiologist checks to make sure that it's correct.
What are the four categories of breast density?
Breast density — The four levels
Breast density — The four levels
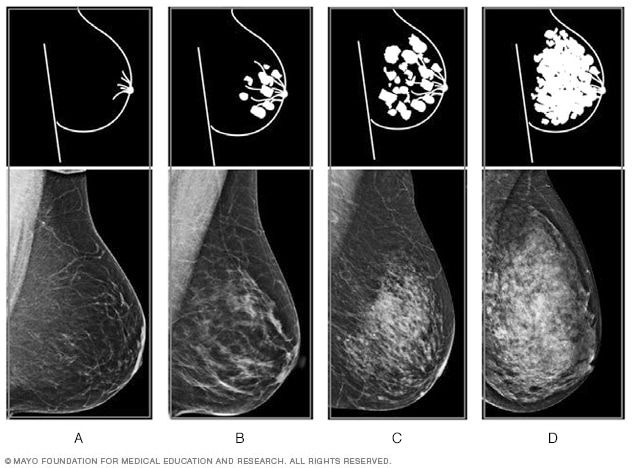
Breast density — The four levels
Mammogram results often include information about breast density. Healthcare professionals use the Breast Imaging Reporting and Data System to report breast density. According to this system, the levels of density are (from left to right) A: almost entirely fatty, B: scattered areas of fibroglandular density, C: heterogeneously dense and D: extremely dense.
Levels of density are described using the American College of Radiology's Breast Imaging Reporting and Data System, which is sometimes shortened to BI-RADS. The levels of density are often included in a mammogram report using letters. The levels of density are:
- A: Almost entirely fatty means that the breasts are almost entirely made up of fatty tissue. There is very little dense breast tissue.
- B: Scattered areas of fibroglandular density means the breasts are mostly made up of fatty tissue. But there are some scattered areas of dense breast tissue.
- C: Heterogeneously dense means that most of the breast tissue is dense breast tissue. But there are some areas of fatty tissue.
- D: Extremely dense means that nearly all of the breast tissue is dense breast tissue. There is very little fatty tissue.
In general, you're considered to have dense breasts if your mammogram report says you have heterogeneously dense or extremely dense breasts. About half of people having screening mammograms have dense breasts.
What causes breasts to become dense?
It's not clear why some people have a lot of dense breast tissue and others do not.
You may be more likely to have dense breasts if you:
- Are younger. Breast tissue tends to become less dense as you get older. But this doesn't happen in everyone. It's possible for dense breasts to happen at any age.
- Have a lower body mass index. Having less body fat makes it more likely that you'll have less fatty tissue and more dense tissue in your breasts.
- Take hormone therapy for menopause. Taking combination hormone therapy to relieve menopause symptoms makes dense breasts more likely.
How serious is dense breast tissue?
Dense breast tissue is a common finding. It doesn't mean there's something wrong. But having dense breasts can affect you in two ways:
- Increases the chance that breast cancer might be missed on a mammogram. Dense breast tissue is harder to see through on a mammogram image. Having dense breasts may increase the chance that something concerning isn't detected on a mammogram.
- Increases the risk of breast cancer. If you have dense breasts, your risk of breast cancer is modestly higher than someone who doesn't have dense breasts. The level of risk is thought to be similar to the risk of breast cancer in someone who has a relative who had the disease. On its own, having dense breast tissue doesn't give you a high risk of breast cancer. Also, having dense breasts does not increase the risk of dying of breast cancer.
How often should I get a mammogram if I have dense breasts?
In general, healthcare professionals recommend that women with an average risk of breast cancer begin screening with mammograms at age 40. For most, the screening should be repeated every year.
Having dense breasts can make it harder to detect cancer on a mammogram. But mammograms are still effective for breast cancer screening if you have dense breasts. Mammograms have been proved to reduce the risk of dying of breast cancer.
Newer mammogram technology gives healthcare professionals more detailed views of breast tissue. This may help improve the chances that cancer will be detected. For instance, nearly all mammogram machines in the United States make digital pictures instead of film pictures. Digital pictures let health professionals zoom in to take a close look at anything concerning.
Additionally, most healthcare facilities in the United States offer 3D mammograms. A 3D mammogram uses computers to combine X-ray pictures of the breast into a 3D image. The 3D images allow healthcare professionals to see past areas of density to look for anything concerning in the breast tissue.
Still, because there is an increased risk of breast cancer in dense breasts, you and your healthcare team might consider other tests.
Is ultrasound better for dense breasts?
There's some evidence that additional tests, such as ultrasound and MRI, may make it more likely that breast cancer is detected in dense breasts. There also is concern that tests such as ultrasound and MRI may find things that need additional testing but are later found to not be cancer. This is called a false-positive result. More research is needed to know which test is best. None of the other tests has been proved to reduce the risk of dying of breast cancer.
You and your healthcare professional may consider additional testing based on your other risk factors and your personal preferences.
Additional tests that might be used in those with dense breasts include:
- 3D mammogram. A 3D mammogram, also called breast tomosynthesis, uses X-rays to take pictures of the breast from many angles. A computer then puts the images together. This makes a 3D image of the breast tissue.
- Breast MRI. Breast MRI uses a magnetic field and radio waves to make 3D images of the breast tissue. It's often recommended for those with a very high risk of breast cancer.
- Breast ultrasound. Ultrasound uses sound waves to make images of structures in the body. It shows the difference between solid masses and sacs filled with fluid, called cysts. Solid masses may be a sign of cancer. A diagnostic breast ultrasound is commonly used to take a closer look at areas of concern detected on a mammogram.
- Contrast-enhanced digital mammogram. A contrast-enhanced digital mammogram uses contrast material that contains iodine. The contrast material can highlight possible areas of concern on a mammogram. The contrast material goes into a vein in your arm. You wait a few minutes for the contrast to reach the breast tissue. Then you have a mammogram.
- Molecular breast imaging. Molecular breast imaging uses a radioactive tracer and a special camera to make pictures of the breast tissue. The tracer has special material in it to help find areas that may have cancer. The special camera detects any tracer that goes to the breast tissue.
Every test has pros and cons. Talk about the options with your healthcare team. Together you can decide which tests are best for you based on your personal risk factors for breast cancer.
March 09, 2024
- AskMayoExpert. Breast cancer screening and options for supplemental screening in the dense breast (adult). Mayo Clinic; 2022.
- Freer PE, et al. Breast density and screening for breast cancer. https://www.uptodate.com/contents/search. Accessed Feb. 5, 2024.
- BI-RADS atlas — Reporting system. American College of Radiology. https://www.acr.org/Clinical-Resources/Reporting-and-Data-Systems/Bi-Rads. Feb. 5, 2024.
- Dense breasts: Answer to commonly answered questions. https://www.cancer.gov/types/breast/breast-changes/dense-breasts. Accessed Feb. 7, 2024.
- Breast cancer screening and diagnosis. National Comprehensive Cancer Network. https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1421. Accessed Feb. 5, 2024.
- MQSA national statistics. U.S. Food & Drug Administration. https://www.fda.gov/radiation-emitting-products/mqsa-insights/mqsa-national-statistics. Accessed Feb. 6, 2024.
- Expert Panel on Breast Imaging. Supplemental breast cancer screening based on breast density. Journal of the American College of Radiology. 2021; doi:10.1016/j.jacr.2021.09.002.
Advertisement
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
Advertising & Sponsorship
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press.
.