Bladder control: Lifestyle strategies ease problems
Simple lifestyle changes may improve bladder control or help medicine work better. Find out what to do to help with bladder control.
By Mayo Clinic Staff
Bladder control problems, such as leaking urine, are common. Fortunately, there are simple ways to improve bladder control and quality of life.
These lifestyle changes work and are safe and easy. They cost little or nothing. Try them before trying other types of treatment, such as medicines or surgery. Or use them with other treatments.
Focus on fluids and food
Fluids and certain foods can affect the bladder.
Too much fluid
Everyone needs to drink enough fluid, but too much can make bladder problems worse. How much you need to drink depends on your health, your activities and where you live.
For those who get up several times at night to urinate:
- Drink more fluids in the morning and afternoon, not at night. Stop drinking a few hours before bedtime.
- Skip alcohol. Limit drinks with caffeine, such as coffee, tea and cola. They can cause you to urinate more.
- Know that foods such as soup add to the total amount of fluids.
Too little fluid
Drinking too little fluid can cause body waste products to build up in urine. The waste products can cause urine to be dark yellow with a strong smell. The buildup can irritate the bladder and increase the need to go.
Bladder irritants
Certain foods and beverages might irritate the bladder, including:
- Coffee, tea and drinks with bubbles, even without caffeine.
- Alcohol.
- Chocolate.
Avoid these possible bladder irritants for about a week to see if symptoms improve. Then gradually — every 1 to 2 days — add one back into the diet. Note changes in how often you urinate.
Changing eating habits might not mean that you can never have favorite foods and drinks. Simply having them less often might help.
Try bladder training
People with bladders that are overly active get used to urinating often or at the slightest urge. Some might visit the toilet to keep from having an accident even when there's no need to use the toilet.
After a while, the bladder signals the brain it's full when it's not. That creates the urge to urinate.
Bladder training involves changing habits. It means going to the toilet at set times, even when there's no urge to urinate. If the times between urinating increase little by little, the bladder fills more fully. This helps control the urge to urinate.
A bladder-training program often follows these basic steps:
- Find the pattern. Keep a diary for a few days. Jot down every time you urinate. A health care provider can use this diary to help you make a schedule for bladder training.
-
Wait longer before urinating. Your bladder diary can tell you how long you wait between urinating. Add on 15 minutes. If you usually urinate every hour, try to wait for an hour and 15 minutes.
Little by little, increase the time between trips to the toilet until you can wait 2 to 4 hours between trips. Increasing the time slowly gives the best chance for success.
-
Stick to the schedule. Once you've made a schedule, do your best to stick to it. Urinate right after waking up in the morning. And urinate each scheduled time even if you have no urge to go.
If you have an urge but it's not time to go, try to wait. Distract yourself or use ways to relax, such as deep breathing. If you feel you're going to have an accident, go to the toilet. But then return to the schedule.
Don't give up if you don't succeed the first few times. Keep trying. Your control is likely to increase.
Strengthen your pelvic floor
Female pelvic floor muscles
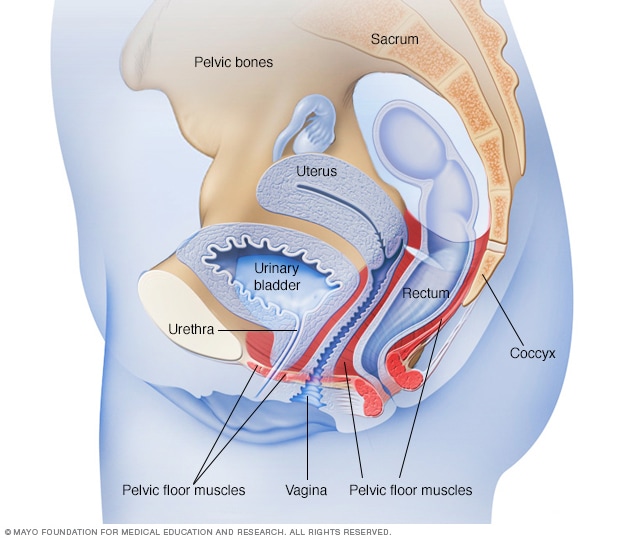
Female pelvic floor muscles
The pelvic floor muscles support the pelvic organs. Those organs include the uterus, bladder and rectum. Kegel exercises can help strengthen the pelvic floor muscles.
Male pelvic floor muscles
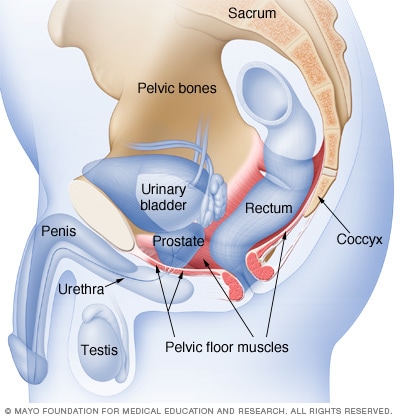
Male pelvic floor muscles
The male pelvic floor muscles support the bladder and bowel and affect sexual function. Kegel exercises can help strengthen these muscles.
Pelvic floor muscles help control urinating. Regularly doing pelvic floor exercises, can strengthen these muscles.
The pelvic floor muscles open and close the tube, known as the urethra, that carries urine from the bladder out of the body. These muscles also hold the bladder up during walking, standing, lifting and sneezing.
To strengthen pelvic floor muscles:
- Practice pelvic floor exercises, also known as Kegel exercises. Squeeze the pelvic floor muscles as though trying to stop the flow of urine for three seconds. Relax for a count of three and repeat several times. Do a set of these exercises three or four times a day. Do them lying down, sitting and standing.
To be sure to do them right, ask your health care provider to guide you. Or ask to see a physical therapist who knows about pelvic floor exercises.
- Biofeedback. Biofeedback can help train pelvic floor muscles. Sensors placed near the muscles send information to a computer about how hard the muscles are working. The information shows on the computer screen.
Seeing that you're using the right muscles might help you with Kegel exercises. Some biofeedback can be done at home.
-
Vaginal weights. Cone-shaped weights are another option to help with Kegel exercises. You place a weight in your vagina. Then you tighten your pelvic floor muscles to keep the weight from falling out.
Many cones come in sets of different weights. So you can build up to heavier weights as your pelvic floor muscles get stronger.
Other factors
Certain medicines, excess weight, smoking and physical inactivity can play a part in bladder control problems. The following can help with bladder control:
- Manage medicines. High blood pressure medicines, heart medicines, water pills, muscle relaxants, antihistamines, sedatives and antidepressants all can play a part in bladder control problems. If you can't hold your urine or can't urinate while taking these drugs, talk to your health care provider.
- Maintain a healthy weight. Being overweight can affect bladder control. Extra body weight puts pressure on the stomach and bladder. This can cause leaking. Losing weight might help.
- Stop smoking. Smokers are more likely to have bladder control problems and to have worse symptoms. Heavy smokers also tend to cough. Coughing can put more pressure on the bladder and make it harder to control. If you cough a lot for any reason, ask your health care provider about treatments.
- Try to avoid constipation. Straining during bowel movements can damage the pelvic floor. Unfortunately, some medicines used to treat bladder control problems can make constipation worse. To improve constipation, exercise, drink enough water and eat high-fiber foods, such as lentils, beans, vegetables and fruits.
Your role in treatment
Behavior therapies take time and practice. But if you stick with the program, you'll likely see your symptoms get better. If these approaches don't work, talk with your health care provider about trying another approach.
May 10, 2025
- Urinary incontinence. Office on Women's Health. https://www.womenshealth.gov/a-z-topics/urinary-incontinence. Accessed Nov. 28, 2022.
- Bladder control problems in women (urinary incontinence). National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/urologic-diseases/bladder-control-problems. Accessed Nov. 28, 2022.
- Lukacz ES. Female urinary incontinence: Treatment. https://www.uptodate.com/contents/search. Accessed Nov. 28, 2022.
- Dumoulin C, et al. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women (Review). Cochrane Database of Systematic Reviews. 2018; doi:10.1002/14651858.CD005654.pub4.