Diagnosis
Tests and procedures used to diagnose Hurthle cell cancer include:
- Physical exam. Your health care provider will examine your neck, checking the size of the thyroid and seeing whether the lymph nodes are swollen.
- Blood tests. Blood tests may reveal changes in your thyroid function that give your provider more information about your condition.
- Imaging tests. Imaging tests, including ultrasound and CT, can help your provider determine whether a growth is present in the thyroid.
-
Examining the vocal cords (laryngoscopy). In a procedure called laryngoscopy, your provider can visually examine your vocal cords by using a light and a tiny mirror to look into the back of your throat. Or your provider may use fiber-optic laryngoscopy. This involves inserting a thin, flexible tube with a tiny camera and light through your nose or mouth and into the back of your throat. Then your provider can watch the motion of your vocal cords as you speak.
This procedure might be recommended if there's a risk that the cancer cells have spread to the vocal cords, such as if you have voice changes that are concerning.
- Removing a sample of thyroid tissue for testing (biopsy). During a thyroid biopsy, a fine needle is passed through the skin of the neck guided by ultrasound images. The needle is attached to a syringe, which withdraws a sample of thyroid tissue. In a laboratory, the sample is examined for signs of cancer by experts trained in analyzing blood and body tissue (pathologists).
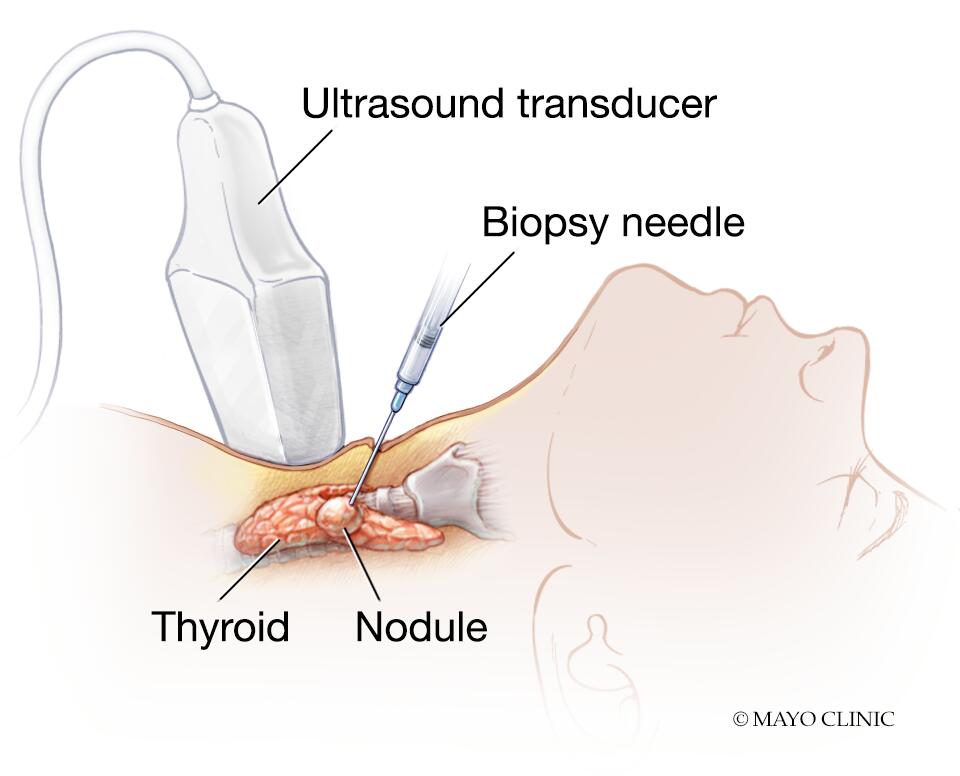
Needle biopsy
During needle biopsy, a long, thin needle is inserted through the skin and into the suspicious area. Cells are removed and analyzed to see if they are cancerous.
Treatment
Treatment for Hurthle cell cancer usually involves surgery to remove the thyroid. Other treatments may be recommended, depending on your situation.
Surgery
Total or near-total removal of the thyroid (thyroidectomy) is the most common treatment for Hurthle cell cancer.
During thyroidectomy, the surgeon removes all or nearly all of the thyroid gland and leaves tiny edges of thyroid tissue near small adjacent glands (parathyroid glands) to lessen the chance of injuring them. The parathyroid glands regulate the body's calcium level.

Parathyroid glands
The parathyroid glands lie behind the thyroid. They produce parathyroid hormone, which plays a role in regulating the body's blood level of calcium and phosphorus.
Surrounding lymph nodes may be removed if there's suspicion that the cancer has spread to them.
Risks associated with thyroidectomy include:
- Injury to the nerve that controls the voice box (recurrent laryngeal nerve), which could cause temporary or permanent hoarseness or a loss of the voice
- Damage to the parathyroid glands, which might require medications to regulate your blood calcium levels
- Excessive bleeding
After surgery, your health care provider will prescribe the hormone levothyroxine (Synthroid, Unithroid, others) to replace the hormone produced by the thyroid. You'll need to take this hormone for the rest of your life.
Radioactive iodine therapy
Radioactive iodine therapy involves swallowing a capsule that contains a radioactive liquid.
Radioactive iodine therapy may be recommended after surgery because it can help destroy any remaining thyroid tissue, which can contain traces of cancer. Radioactive iodine therapy may also be used if Hurthle cell cancer has spread to other parts of the body.
Temporary side effects of radioiodine therapy can include:
- Dry mouth
- Decrease in taste sensations
- Neck tenderness
- Nausea
- Fatigue
Radiation therapy
Radiation therapy uses high-powered energy beams, such as X-rays or protons, to kill cancer cells. During radiation therapy, you're positioned on a table and a machine moves around you, delivering the radiation to specific points on your body.
Radiation therapy may be an option if cancer cells remain after surgery and radioactive iodine treatment or if Hurthle cell cancer spreads.
Side effects may include:
- Sore throat
- Sunburn-like skin rash
- Fatigue
Targeted drug therapy
Targeted drug treatments use medications that attack specific weaknesses within cancer cells. Targeted therapy may be an option if your Hurthle cell cancer returns after other treatments or if it spreads to distant parts of your body.
Side effects depend on the particular drug, but may include:
- Diarrhea
- Fatigue
- High blood pressure
- Liver problems
Targeted drug therapy is an active area of cancer research. Doctors are studying many new targeted therapy drugs for use in people with thyroid cancer.
Get Mayo Clinic cancer expertise delivered to your inbox.
Coping and support
A diagnosis of Hurthle cell cancer can be challenging. Many people feel stressed and anxious. With time you'll find strategies to cope. Until then, here are some ideas that might help:
- Find someone to talk with. You may feel comfortable discussing your feelings with a friend or family member, or you might prefer meeting with a formal support group. Support groups for the families of cancer survivors also are available.
- Let people help. Cancer treatments can be exhausting. Let friends and family know what would be most useful for you.
- Set reasonable goals. Having goals helps you feel in control and can give you a sense of purpose. But choose goals that you can reach. Write down a list of priorities each day and recognize that you can't do it all.
- Conserve your energy. Recognize that you can say no to demands and expectations that will reduce your energy. Save your energy for doing the things that are most important to you.
- Take time for yourself. Eating well, relaxing and getting enough rest may help combat the stress and fatigue of cancer.
Preparing for your appointment
Start by making an appointment with your health care provider if you have signs and symptoms that worry you.
If Hurthle cell cancer is suspected, you may be referred to a doctor who specializes in treating thyroid disorders (endocrinologist) or a doctor who specializes in treating cancer (oncologist).
Because appointments can be brief, it's often helpful to arrive well prepared. Here's some information to help you get ready and what to expect from your provider.
What you can do
- Write down your symptoms, including any that may seem unrelated to the reason why you scheduled the appointment.
- Write down your key medical information, including other conditions.
- Make a list of all your medications, including prescriptions and medicines that are available without a prescription, as well as any vitamins or supplements that you take.
- Gather information about your family health history, including thyroid diseases and other diseases that run in your family.
- Ask a relative or friend to accompany you to help you remember what the provider says.
- Write down questions to ask your provider.
- Ask how to access your provider's online patient portal so you can see what the provider has written in your medical history. There may be some technical terminology, but it can be helpful to review what was shared during your appointment.
Questions to ask your doctor
- What's the most likely cause of my symptoms? Are there other possible causes?
- What kinds of tests do I need? Do they require any special preparation?
- What treatments are available, and what side effects can I expect?
- What's my prognosis?
- How often will I need follow-up visits after I finish treatment?
- I have other health conditions. How can I best manage them together?
- What happens if I choose not to have treatment?
What to expect from your doctor
Your provider is likely to ask you a number of questions. Being ready to answer them may leave time to go over points you want to spend more time on. You may be asked:
- When did you first begin experiencing symptoms? Have they been continuous or occasional?
- Have your symptoms gotten worse?
- Do you have a personal or family history of cancer? What type?
- Have you ever received radiation treatments to the head or neck area?