July 27, 2022
Reticular pseudodrusen (RPD), basal laminar drusen (BLD) and especially calcified drusen (CaD) were associated strongly with advanced age-related macular degeneration (AMD) in a cross-sectional study of a large group of eye-bank eyes selected from a population at risk of AMD.
高风险黄斑
高风险黄斑
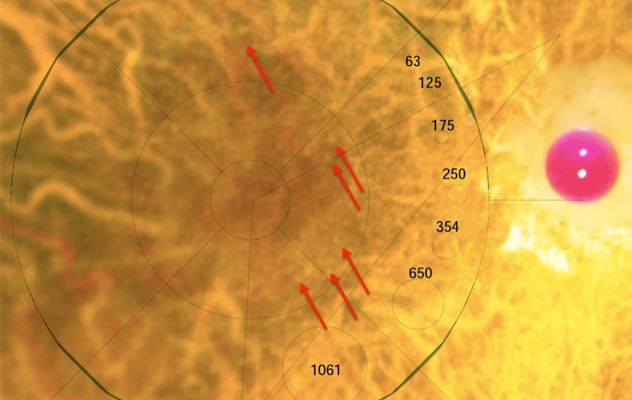
这是一位死于冠状动脉疾病(心脏病发作)的眼库捐献者的眼睛后部(后极)彩色图像。图片由 Lions Eye Institute for Transplant and Research 提供。
"AMD is a leading cause of blindness in many diverse, global populations. No treatments currently exist for geographic atrophy (dry AMD) or unresponsive exudative AMD (wet AMD). Both are part of end-stage AMD," says Timothy W. Olsen, M.D., an ophthalmologist at Mayo Clinic in Rochester, Minnesota. "Specific drusen phenotypes have been shown to represent diagnostically relevant risk factors for progression to advanced stages of AMD. Our intent in this study was to stage maculopathy, assess and quantify drusen, determine drusen subtype frequency, and compare drusen subtypes with age-related AMD stage and cause of death."
The study was published in Ophthalmology Retina in 2021.
Clinical characteristics and evaluation
Eye bank personnel procured donor eyes for research and obtained at-risk donors for AMD by prioritizing eyes of donors over 65 years old. Dr. Olsen and eye bank personnel recorded donor characteristics including age, race, sex, and time and cause of death, along with a limited medical and ocular history. Globes were procured at a mean of 12 hours after donor death.
Researchers used the Minnesota Grading System (MGS) to obtain images from 2,092 eye bank eyes donated by 1,067 donors between January 2005 and August 2020. Ultimately, 1,777 eyes formed the database and both the four-step and nine-step MGS criteria were applied.
The four-step MGS criteria are based on drusen size, type of drusen, presence of pigmentary changes, and geographic atrophy or exudative AMD, or both. The four steps indicate disease-free versus early, intermediate and advanced stages of AMD. "The nine-step MGS criteria allow for more granular AMD staging by quantifying total drusen area, pigmentary changes and areas of atrophy," says Dr. Olsen. "The MGS links directly the Age-Related Eye Disease Study, or AREDS, the largest human database on AMD progression, and thus translates clinical risk to MGS score." The Age-Related Eye Disease Study was published in the American Journal of Ophthalmology in 2001.
Researchers analyzed the association between each drusen subtype group and known cause of death, tabulated per person and classified as cardiovascular, neoplastic, infectious (such as pneumonia) and other (such as renal failure, intestinal bleeding or trauma).
In both the four-step and nine-step MGS, eyes with each drusen subtype were associated independently and significantly with more-advanced stages of AMD:
- RPD frequency was 13% (228 eyes); mean donor age was 80 years
- BLD frequency was 7% (131 eyes); mean donor age was 80 years
- CaD frequency was 5% (84 eyes); mean donor age was 84 years
CaD was more prevalent in older donors (80 years older on average) and showed a strong association with advanced disease.
"Our laboratory established the four-step and nine-step MGS. Both use the specific phenotype definitions from the AREDS applied to eye-bank eyes," notes Dr. Olsen. "A key advantage of using an eye bank model is that postmortem eyes also can be graded for the presence of visible RPD, BLD and CaD, thus allowing determination of associations for each entity with AMD stage and cause of death." The AREDS includes more than 70 publications that characterize the clinical course of AMD from living patients.
RPD and cardiovascular death
"We found that RPD, BLD and CaD all showed a strong association with more-advanced stages of AMD, but interestingly, we also identified a potential association of RPD and cardiovascular death," says Dr. Olsen. "We propose a mechanistic hypothesis for such an association: RPD may represent an ophthalmologic biomarker for coronary artery disease.
"Our prior studies, which used cytologic analysis of MGS-graded donor tissue at the National Institutes of Health, have shown a similar chronic inflammatory pathway, possibly involving tissue macrophage polarization — either primary or secondary — that may be involved in the development of pathologic vascular endothelial plaques in coronary artery disease, as well as in the generation of RPD."
For more information
Mano F, et al. Association of drusen phenotype in age-related macular degeneration from human eye-bank eyes to disease stage and cause of death. Ophthalmology Retina. 2021;5:743.
The Age-Related Eye Disease Study Research Group. The age-related eye disease Study system for classifying age-related macular degeneration from stereoscopic color fundus photographs: The Age-Related Eye Disease Study Report Number 6. American Journal of Ophthalmology. 2001;132:668.
Refer a patient to Mayo Clinic.