Nov. 19, 2021
J. (Nick) Nicholas Warner, M.D., a urologist at Mayo Clinic in Rochester, Minnesota, specializes in reconstructive urology and benign prostatic hyperplasia surgery. Dr. Warner and his team have recently added bipolar enucleation of the prostate to the armamentarium of treatments for benign prostatic hyperplasia.
What is enucleation of the prostate?
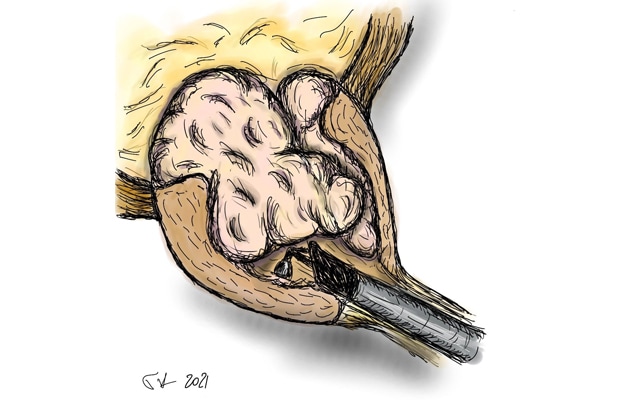
Enucleation of the prostate is the process of removing the adenoma of the prostate within the prostatic capsule. There are several different ways to perform a prostate enucleation:
- Through a large open incision (simple prostatectomy)
- Robotically with small incisions
- Through the urethra (transurethral), without any incisions
How did transurethral enucleation become a preferred operation for enlarged prostates?
The first transurethral enucleation was performed in 1983 in Japan. It's challenge, however, was that once the tissue was freed from the prostate, an incision still had to be made to remove the tissue. It was not until the advent of the morcellator in the late '90s that the operation gained more attention. The morcellator allows the pieces of adenoma to be removed through the urethra.
Enucleación transuretral
Enucleación transuretral
La enucleación de la próstata se hace a través de la uretra, sin incisiones.
There are obvious benefits of transurethral enucleation. First, there are no incisions. Second, the operation can be performed on any size prostate. Third, in most cases we can remove the catheter the day after the operation. Other types of prostate surgery may require a catheter be inserted for longer, such as seven days. Finally, enucleation is a complete removal of the adenoma, giving the longest-lasting results compared with other surgical options, such as transurethral resection of the prostate.
Transurethral enucleation can be performed with a number of different energy sources, including a holmium laser, usually called holmium laser enucleation of the prostate (HoLEP) or with bipolar energy, usually called bipolar enucleation of the prostate (BipolEP).
The end product is the same with either HoLEP therapy or BipolEP therapy, but the learning curve and equipment costs of BipolEP are more favorable.
What type of patient is particularly well suited for BipolEP?
The ideal patient for bipolar enucleation will have a larger prostate, usually over 80 mL in size, or be in urinary retention. In either situation, the enucleation procedures have shown to be most effective. In my opinion, smaller prostates deserve smaller operations. A number of good minimally invasive therapies are available for patients with smaller prostates. Patients who have been told they will not be able to urinate on their own without a catheter or who have been offered an open surgery because their prostates are "too big" are good candidates for BipolEP.
What are the side effects of BipolEP?
The side effect profile of BipolEP is generally quite mild, especially when compared with other possible interventions. However, patients with smaller prostates do have a higher rate of scar tissue formation after surgery. This scar tissue can form either at the junction of the bladder and the prostate, or along the urethra.
Another risk after this operation is urinary incontinence. While long-term the risk is very low, it is not unusual to have some leakage with activity for a few months after the surgery. Bleeding risk and infection are both very rare. While the operation does not affect erections, or the ability to achieve orgasm, most men will lose the ability to ejaculate after the surgery.
What is the typical recovery?
Most men will keep their Foley catheter inserted just overnight. The catheter will be removed the following morning and patients complete a voiding trial. We ask patients to limit strenuous physical activity over the next two weeks and drink plenty of fluids to keep the urine a light, clear color. After two weeks, patients are cleared to resume regular activity but are cautioned that they may still see occasional bits of tissue or bleeding with heavy activity.
If men do experience urinary incontinence, it tends to improve over the first three months. In addition, if men had, preoperatively, a lot of urinary issues — such as urinary frequency, urgency or nocturia — these issues may worsen for a few weeks after surgery, before they start to improve.