June 09, 2023
Plantar fasciopathy (PF), known by some as plantar fasciitis, is a common condition affecting the fibrous tissue that runs along the bottom of the foot. The primary symptom is medial heel pain when weight bearing. Typically, heel pain caused by PF is most intense with the first few steps in the morning. Pain also can occur after long periods of standing or walking, or at the end of the day.
Risk factors and diagnosis
Although this condition can affect adults at any age, the peak incidence of PF is between 40 and 60 years of age.
"We often see plantar fasciopathy develop when the foot is subjected to increased load or has reduced shock absorption capability," explains Marianne T. Luetmer, M.D., a physiatrist at Mayo Clinic in Rochester, Minnesota. "Onset of this condition is often associated with changes in an exercise program, exercise surface or footwear."
Risk factors for PF include:
- Obesity and pregnancy, due to extra stress on the plantar fascia.
- Activities that involve prolonged walking or standing on hard surfaces, and those that stress the heel, such as running.
- Biomechanical issues that adversely affect the way weight is distributed while standing, including overpronation, reduced ankle dorsiflexion, tight posterior chain, proximal muscle weakness.
- Inflammatory conditions.
Dr. Luetmer notes that in general, the diagnosis can be established through history and physical examination. X-rays and other imaging are not typically required unless other causes of pain, such as a stress fracture, are suspected. Ultrasound is used to evaluate for and plan interventions.
Conservative management
As with other musculoskeletal conditions, PF can respond to rest, ice, and activity or training modifications. Dr. Luetmer notes that addressing skeletal alignment and biomechanics, and providing soft tissue manual therapy can sometimes be beneficial. Additional initial management approaches can include any of the following:
- Exercises to improve intrinsic foot strength and/or aponeurosis loading as guided by physical therapy, although optimal methods remain unknown.
- Shoe modifications, trial of a heel cup or orthotics as needed.
- Splinting at night to prevent passive contracture.
- Shock wave therapy, although available evidence for this is mixed and of low quality.
Interventions
When conservative treatment measures fail to relieve PF symptoms, multiple additional interventions are available. Researchers have examined the efficacy of some of these interventions, but Dr. Luetmer stresses that additional high-quality study data are needed to help identify which methods or combination of methods yields the best long-term outcomes.
-
Ultrasound-guided corticosteroid injections (CSIs) and platelet-rich plasma (PRP) injections
According to Dr. Luetmer, published data related to the use of these therapies to treat PF have some limitations.
"It's difficult to find accurate data related to the risk of plantar fascia rupture, fat pad atrophy and other adverse effects that are associated with corticosteroid injections. Until more long-term data are available, the general recommendation is to limit the use of CSIs to 1 to 2 injections to provide short-term pain relief," explains Dr. Luetmer.
Some small studies with low to moderate quality data comparing CSI with PRP suggest that patients who were treated with PRP, followed by protected weight bearing and physical therapy, experienced better pain relief and function at three, six and 12 months after treatment.
"Multiple studies suggest that platelet-rich plasma injections may take longer to provide pain relief than corticosteroid injections, but the impact of platelet-rich plasma appears to be longer lasting," says Dr. Luetmer. Studying this is challenging since in many cases, ultrasound-guided percutaneous needle tenotomy is performed in conjunction with the PRP injection. Thus, researchers do not know which component — the tenotomy, the PRP or the combination — is most beneficial.
Tenotomía/fasciotomía percutánea ultrasónica
Tenotomía/fasciotomía percutánea ultrasónica
El objetivo de este procedimiento es eliminar el tejido degenerativo y promover la cicatrización. Cuando va seguido de un soporte de peso protegido y un protocolo específico de fisioterapia, ha demostrado ser prometedor como tratamiento de la fasciopatía plantar.
-
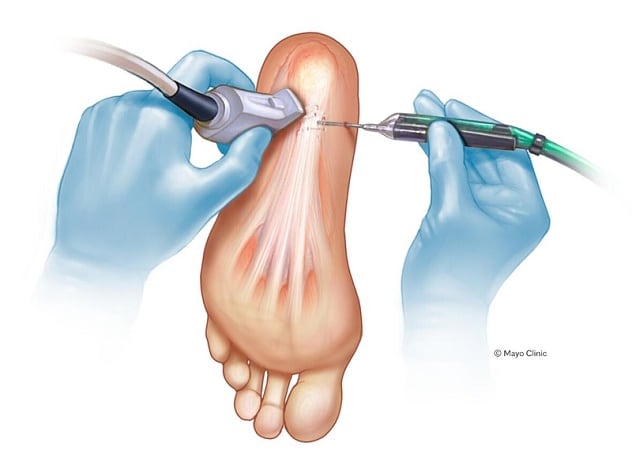
Percutaneous ultrasonic tenotomy/fasciotomy and debridement
The goal of this procedure is to remove degenerative tissue and promote healing. When followed by protected weight bearing and a specific physical therapy protocol, it has shown promise as a treatment for PF.
"A recent study presented by Mayo colleagues at the 2023 American Medical Society for Sports Medicine Annual Meeting demonstrated high patient satisfaction in a small population of patients an average of six years post-procedure. However more high-quality data are needed to establish optimal timing and candidates for the procedure as well as long-term efficacy," says Dr. Luetmer.
-
Dextrose injections (prolotherapy)
According to Dr. Luetmer, the exact mechanism of this treatment is unknown, and published studies have yielded mixed data on its efficacy specific to PF.
"Plantar fasciopathy is a common yet often challenging diagnosis to manage, and quality evidence regarding optimal treatment methods is lacking. For symptoms that are refractory to conservative management, Mayo physiatrists are expanding the use of percutaneous ultrasonic tenotomy/fasciotomy and debridement, as well as PRP, to offer minimally invasive and longer term treatment options."
For more information
Ha C, et al. Long-term outcomes of ultrasound-guided percutaneous fasciotomy and debridement for chronic plantar fasciopathy. Presentation at: American Medical Society for Sports Medicine Annual Meeting; 2023; Phoenix, Ariz.
Refer a patient to Mayo Clinic.