Sept. 18, 2025
Precision medicine is transforming how Mayo Clinic Children's cares for children with serious or rare diseases. By combining rapid whole-genome sequencing (rWGS), artificial intelligence (AI) and functional omics, the new BabyFORce program enables Mayo Clinic clinicians to move from diagnosis to personalized treatment — potentially uncovering therapeutic options where none previously existed. This innovative approach is already changing lives in the NICU, offering targeted therapies for infants with rare genetic conditions during a critical window of development.
 Precision medicine in the NICU
Precision medicine in the NICU
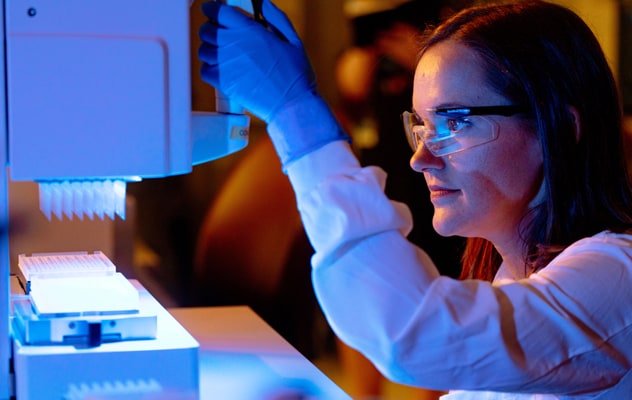
Rapid whole-genome sequencing, paired with AI, is accelerating the diagnosis and treatment of rare diseases.
"Offering rapid whole-genome sequencing has been a clinical standard practice in our neonatal intensive care unit (NICU) since June 2022," says Whitney S. Thompson, M.D., M.Phil., a fellow in Neonatal Medicine and Clinical Genomics at Mayo Clinic in Rochester, Minnesota. Whole-genome sequencing (WGS) completed in days instead of months has helped the NICU streamline the diagnostic process and avoid unnecessary — and sometimes invasive — testing. "Now, we are taking neonatal care to the next level by using whole-genome sequencing to make diagnoses and AI technology to identify potential therapeutics for our youngest patients," says Dr. Thompson.
One young patient positively affected by Mayo Clinic's genomic advances is Jorie Kraus. She was diagnosed with DeSanto-Shinawi syndrome shortly after birth when rWGS revealed she was missing part of chromosome 10. The diagnosis provided answers for Jorie's family members and helped them anticipate her neurodevelopmental differences, but it did not alter her prognosis.
The catalyst for Jorie has been the development of BabyFORce. This first-of-its-kind initiative, developed at Mayo Clinic and introduced in April 2024, falls under the umbrella of Mayo Clinic's Center for Individualized Medicine. BabyFORce relies on an advanced understanding of functional omics along with AI technology to bridge the gap between diagnosis and treatment for babies such as Jorie who have rare genetic diseases.
"BabyFORce steps in after rapid genome sequencing is complete," says Laura J. Lambert, Ph.D. Dr. Lambert is the director of Mayo Clinic's Functional Omics Resource (FORce) and cocreated BabyFORce with Dr. Thompson. "If genome sequencing identifies a genetic variant, we use that information and leverage AI to help find a potential treatment tailored to the needs of that patient's unique genetic profile," says Dr. Lambert.
Combining rapid WGS with BabyFORce creates the potential for diagnosis and possibly treatment within months — instead of years or decades.
How BabyFORce identifies safe care pathways for infants with genetic conditions
WGS is critical to what BabyFORce does. However, it is just the first step in a complex process that involves:
- Understanding the disease by identifying and analyzing the mechanism that's driving it.
- Identifying the best way to compensate for the genetic variant, such as upregulating or downregulating genetic expression.
- Enlisting AI to analyze the gene variant and treatment goal and create a list of existing compounds that may help.
- Evaluating the list of FDA-approved drugs to eliminate treatments that may be unsafe for children.
- Collecting cells that express the gene and protein, such as skin cells, from the patient.
- Growing the cells in a lab for compound screening and hit validation.
- Testing physiologically relevant drug concentrations on patient-derived cell cultures and analyzing the data to see whether the treatment works.
- Bringing the treatment to the patient and closely monitoring phenotype and side effects.
"A critical part of the process is performing experimental wet lab work using the patient's cells to predetermine whether there will be a response," says Dr. Lambert. "This step provides confidence that there will be a true and significant response before we clinically implement the treatment."
In addition to identifying and testing the treatment, the team works with Mayo Clinic's ethics committees and legal department to ensure the treatment is in the best interest of the patient.
In Jorie's case, the entire process took several months. However, the timeline varies for each specific patient and gene variant.
For Jorie, the wait was worth it. AI identified clonazepam as an FDA-approved drug that might be repurposed to compensate for Jorie's chromosome deletion. The drug was first tested on a sample of Jorie's skin cells, which responded positively to the treatment. After determining the best way to clinically implement the treatment and clearing it ethically and legally, Jorie began treatment. Within one month, blood samples revealed normal gene expression levels, and Jorie showed significant verbal and physical developmental gains.
Critical components of precision medicine in the NICU
WGS can serve as a roadmap for personalized care. The sooner it's completed, the sooner physicians can begin searching for a potential treatment, if one exists.
However, WGS — no matter how quickly it's completed — is not enough on its own. Access to genetic counseling and multidisciplinary collaboration is critical. Neonatal specialists, pharmacists, geneticists and biomedical scientists work together to make care decisions in the best interest of the patient before, during and after genetic testing. Genetic counselors serve as a bridge between the precision medicine team and the family.
"The goal is to provide every patient with a pathway and an understanding of what's next after rWGS," says Dr. Thompson. "BabyFORce and our multidisciplinary approach to neonatal care help us provide options for patients where previously no options existed."
Looking ahead with rWGS and BabyFORce
Mayo Clinic Children's is working toward building a transformative Pediatric Precision Medicine Program to help bring BabyFORce and other innovations to all pediatric patients. The next step for BabyFORce is to use AI to speed up certain parts of the process — specifically the interpretation of genome sequencing and the search for therapeutics.
"Our therapeutics are lagging far behind our diagnostics right now," says Dr. Thompson. "But the approach we use with BabyFORce might make it possible to treat a wide array of diagnoses, including rare diseases and more common conditions. We want all children to have access to that opportunity. We're not there yet, but that's the direction we are going."
For more information
Mayo Clinic's Center for Individualized Medicine.
Refer a patient to Mayo Clinic.