Oct. 20, 2020
Prueba de campo visual
Prueba de campo visual
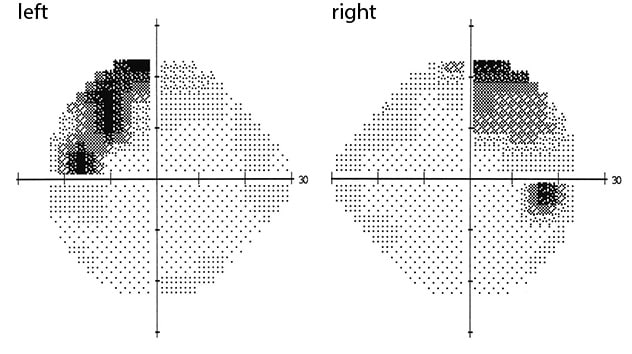
Pruebas de campo visual que confirman cuadrantanopsia bitemporal superior.
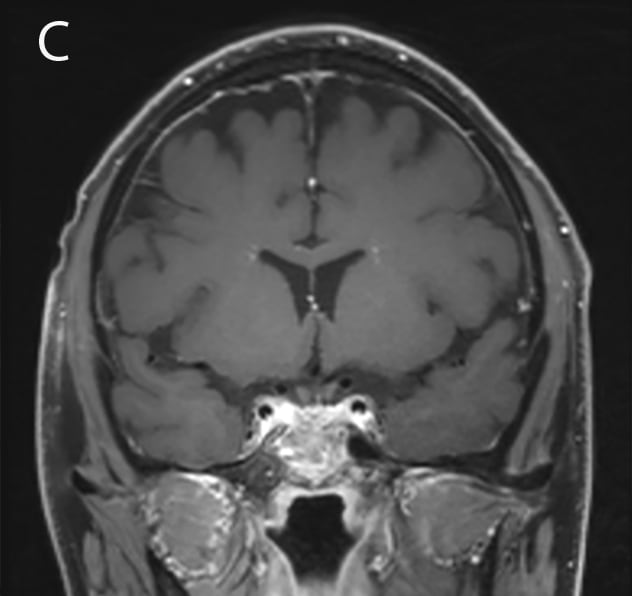
A 44-year-old man with no significant past medical history presented with fatigue and a newly discovered 1.8 cm pituitary mass. He reported a six-month history of progressive fatigue and over the last two months had developed orthostatic hypotension, erectile dysfunction, polyuria and polydipsia. Along with these symptoms, he noted weight loss of 18 pounds, loss of appetite and fevers. The patient also experienced rhinorrhea with clear water-like nasal secretions that did not respond to nasal steroids for the last three weeks. On exam, he appeared ill and fatigued. Visual field testing confirmed a bitemporal superior quadrantanopsia.
Resultados de las pruebas de laboratorio
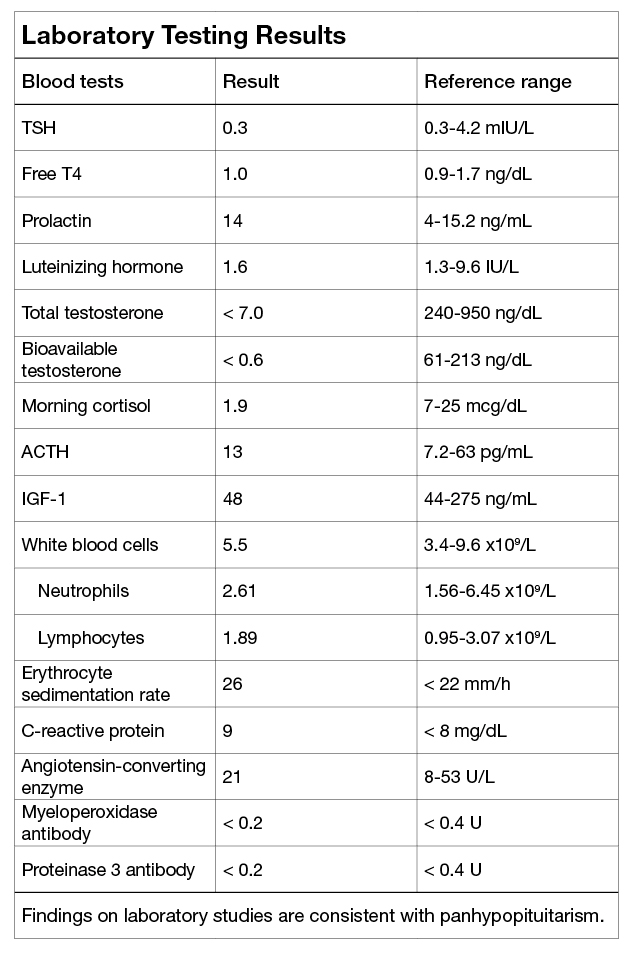
Resultados de las pruebas de laboratorio
Los hallazgos de estudios de laboratorios coinciden con el panhipopituitarismo.
Findings on laboratory studies were consistent with panhypopituitarism.
Presentación inicial de tumor de tejido blando en la región selar
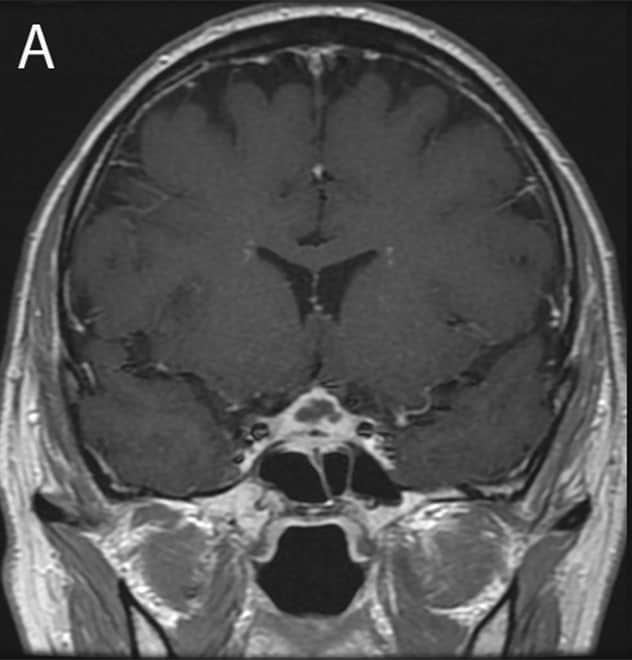
Presentación inicial de tumor de tejido blando en la región selar
Presentación inicial: tumor de tejido blando de 1,8 cm en la región selar, según IRM.
A water deprivation test confirmed central diabetes insipidus. A pituitary-directed head magnetic resonance imaging (MRI) revealed a 1.8 cm soft tissue mass in the sella extending into the suprasellar cistern with distortion of the optic chiasm. The mass appeared heterogeneous with low attenuation in neighboring tissue and thickening of the sphenoid air cells.
The patient received transsphenoidal resection of the pituitary mass. Grossly, the inner portions of the pituitary mass appeared milky and necrotic, concerning for a pituitary abscess. His pathology showed acute and chronic inflammation with no evidence of IgG4 or lymphoproliferative disease. No organisms were noted microscopically, and bacterial and viral cultures of the pituitary material had no growth. An extensive infectious disease work-up was completed with normal results.
Tumor en crecimiento en la región selar a los tres meses
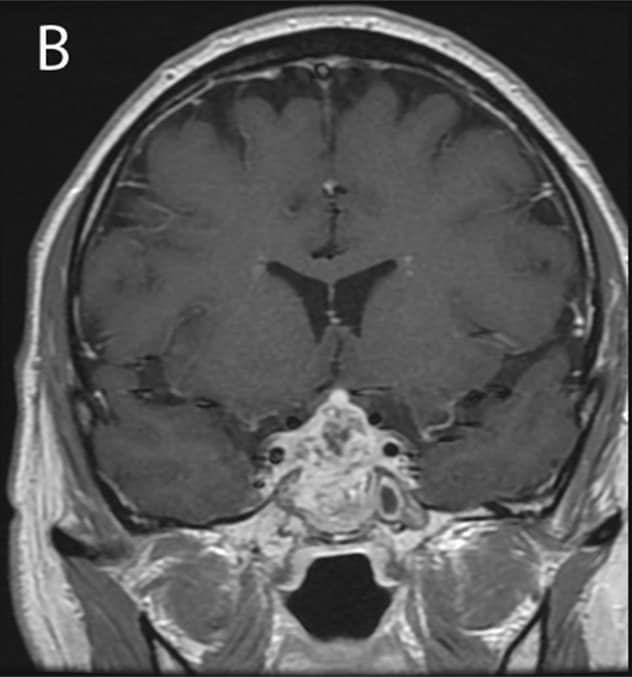
Tumor en crecimiento en la región selar a los tres meses
Tres meses después de la presentación inicial: tumor en desarrollo en la región selar con proliferación en los senos esfenoidales y cavernoso en imágenes por resonancia magnética.
The patient was treated empirically with a course of ertapenem. Three months later, he developed worsening headache, fever, chills and visual changes. MRI showed the pituitary mass was extending into the sphenoid and cavernous sinuses. A pituitary biopsy was inconclusive. Eventually, culture of his cerebrospinal fluid grew Nocardia farcinica approximately one month after collection.
Mejora del tamaño del tumor selar
Mejora del tamaño del tumor selar
El postratamiento con antibioticoterapia dirigida mejora el tamaño del tumor selar, como se muestra en la resonancia magnética.
The patient completed a course of targeted antibiotic therapy with trimethoprim-sulfamethoxazole and linezolid with lasting resolution of his symptoms. MRI showed shrinkage of the pituitary mass.
Discussion
Pituitary adenomas account for the majority of sellar masses. Our case highlights the challenges of diagnosis when a patient presents with a more unusual pathology.
Clinical findings suggestive of a non-adenoma pituitary mass
- Rapid onset of symptoms (for example, over weeks)
- Constitutional symptoms (fever, chills, weight loss)
- Neurological symptoms
- New rhinorrhea, concerning for cerebrospinal fluid leak
- Presence of diabetes insipidus
- Elevated inflammatory markers
- Pituitary mass with peripheral enhancement on magnetic resonance imaging
These are signs and symptoms that suggest a sellar mass may not be a pituitary adenoma. The differential diagnosis includes infectious, inflammatory and neoplastic processes. An extensive laboratory and pathology evaluation may be necessary to confirm the diagnosis.
Pituitary abscess is a rare finding. As noted in research published by Agyei and others in World Neurosurgery in 2017, patients often present with headache and visual symptoms rather than fever. Staphylococcus organisms are the most common cause, but fungal infections can also occur. However, culture testing is often negative, as in this case, and empirical antibiotic therapy is needed. Imaging findings are often similar to pituitary adenomas, but intraoperative findings show purulent material and no evidence of other pathology.
As reported in research published by Carpinteri and others in Best Practice and Research Clinical Endocrinology and Metabolism in 2009 and Esposito and others in Pituitary in 2017, inflammatory and granulomatous processes such as sarcoidosis or vasculitis can also present as pituitary masses and pituitary dysfunction, often including diabetes insipidus. Langerhans cell histiocytosis and Erdheim-Chester disease can have a similar presentation. The majority of these inflammatory processes also cause systemic symptoms at the time of presentation. A neoplastic process can also occur in the sella, such as lymphoma or germ cell tumors. Primary pituitary carcinomas are very rare, as supported by research published by Pernicone and others in Cancer in 1997.
A sellar mass is typically a pituitary adenoma, but rarer diagnoses, such as pituitary abscess, sarcoidosis, vasculitis or lymphoma, should be considered when a patient presents with rapid onset and progression of symptoms, diabetes insipidus, or a heterogeneous pituitary lesion on imaging.
For more information
Agyei JO, et al. Case report of a primary pituitary abscess and systematic literature review of pituitary abscess with a focus on patient outcomes. World Neurosurgery. 2017;101:76.
Carpinteri R, et al. Pituitary tumours: Inflammatory and granulomatous expansive lesions of the pituitary. Best Practice and Research Clinical Endocrinology and Metabolism. 2009;23:639.
Esposito D, et al. Pituitary dysfunction in granulomatosis with polyangiitis. Pituitary. 2017;20:594.
Pernicone PJ, et al. Pituitary carcinoma: A clinicopathologic study of 15 cases. Cancer. 1997;79:804.