Jan. 16, 2026
Monoclonal antibody medication can slow the progression of early Alzheimer's disease. But some patients on those therapies can experience edema or hemorrhagic changes. Mayo Clinic's neuroradiologists have expertise with detecting these amyloid-related imaging abnormalities (ARIA) and managing patient care.
"We have a very regimented schedule of MRI scans for these patients," says John V. Murray Jr., M.D., a neuroradiologist at Mayo Clinic in Jacksonville, Florida. "We collaborate with our Neurology colleagues, incorporating radiographic findings with clinical findings to determine if antiamyloid therapy can be continued safely."
Severe symptoms of ARIA are uncommon but can involve seizures, coma or other focal neurological deficits. More common symptoms include headache, confusion, visual changes, dizziness and nausea. Patients with mild ARIA are sometimes asymptomatic.
Balancing the risks and benefits of continuing antiamyloid therapy requires experience and sound clinical judgment. "We have to look very closely for microhemorrhages and edema on MRI, and to determine if the findings are mild, moderate or severe," says Neetu Soni, M.B.B.S., M.D., a neuroradiologist at Mayo Clinic's campus in Florida. "We want to avoid further complications but also help patients to continue antiamyloid therapy when that's safe."
Multidisciplinary decision-making
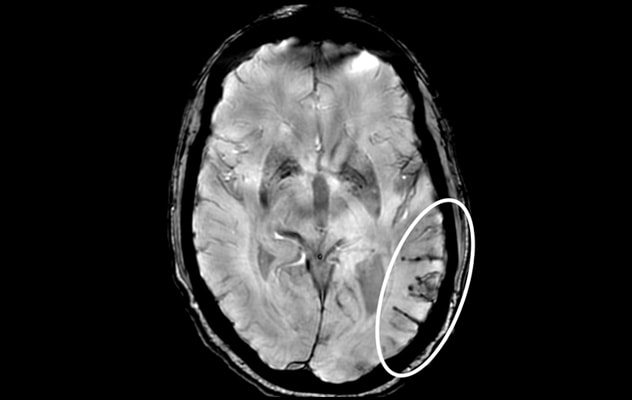 Severe ARIA-H
Severe ARIA-H
Axial T2* gradient echo MRI demonstrates a large area of superficial siderosis and microhemorrhages in the left temporal region (white circle) — resulting in a diagnosis of amyloid-related imaging abnormalities-hemosiderin (ARIA-H).
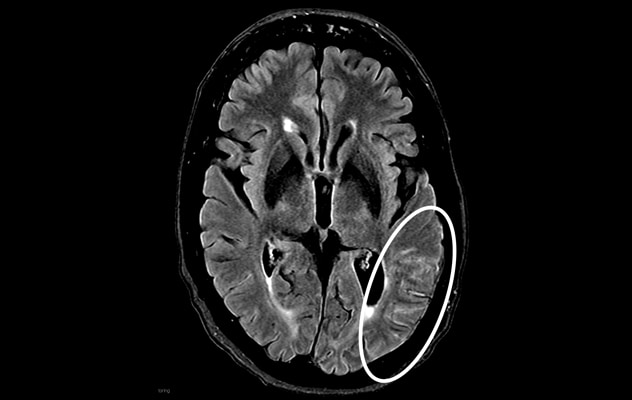 Moderate ARIA-E
Moderate ARIA-E
Axial fluid-attenuated inversion recovery MRI in the same patient shows hyperintense sulcal effusion involving the left temporal region (white circle) — indicating moderate ARIA-edema (ARIA-E). Antiamyloid therapy was discontinued after imaging.
ARIA may involve edema, microhemorrhages and superficial siderosis. The APOE e4 allele is a genetic variant that impacts the risk of ARIA, including severe forms. Patients on blood thinners also face an increased risk of hemorrhage when taking antiamyloid medications.
"Although severe complications aren't common, they can potentially be devasting," Dr. Murray says.
At Mayo Clinic, patients taking these medications have regular MRI scans, with scheduling based on the specific therapy. Imaging and clinical findings are discussed at a conference that includes specialists in neurology as well as neuroradiology and nuclear medicine. "Based on all those findings, we decide whether the therapy can continue," Dr. Soni says.
The multispecialty approach is key. "It's not just a radiologist saying, 'There's a couple of microhemorrhages here,' " Dr. Murray says. "Our combined expertise helps us get the best potential outcome for each patient. Patients with very mild ARIA who are asymptomatic might elect to continue the therapy."
Mayo Clinic is exploring potential enhancements to ARIA imaging, using artificial intelligence software approved by the Food and Drug Administration. The software could potentially lead to improved detection of ARIA.
"Quite often in older patients, we can see lesions that are tiny black dots that are indicative of microhemorrhage. In some patients these may not be clinically significant," Dr. Murray says. "But in this subset of patients on antiamyloid medication, one or two black dots can make a big difference."
Mayo Clinic specialists are committed to providing optimal, safe care to patients with Alzheimer's disease. "We know that these cutting-edge therapies can clear amyloid. They blunt the curve of progression and can give patients a higher quality of life, at least for some time," Dr. Murray says. "We want to do that in the safest way possible. Collaboration with our clinical colleagues is how we do that."
For more information
Refer a patient to Mayo Clinic.