Diagnóstico
Preguntas frecuentes sobre el cáncer de vejiga
Mira el video del Dr. Mark Tyson para conocer las respuestas a las preguntas más frecuentes sobre el cáncer de vejiga.
Hola, soy el Dr. Mark Tyson, urólogo de Mayo Clinic, y estoy aquí para responder a algunas de las preguntas importantes que puedes tener sobre el cáncer de vejiga.
¿Qué tipo de cáncer de vejiga tengo?
El tipo de cáncer de vejiga que se le suele diagnosticar a la mayoría de los pacientes es el carcinoma urotelial. Si bien hay otros tipos de cáncer de la vejiga, como adenocarcinomas y carcinomas celulares pequeños, el carcinoma urotelial es el más frecuente. Algunos carcinomas uroteliales presentan lo que se conoce como histología variante, que incluye la variedad plasmocitoide, micropapilar y microquística. Estos son tumores que, generalmente, aumentan la agresividad del carcinoma urotelial. Además del tipo de célula, también es importante saber el grado y la etapa del tumor. Por lo general, los tumores se clasifican de grado bajo y de grado alto (que son lo más agresivos). El grado, la etapa y el tipo de cáncer se usan para determinar el tipo de tratamiento que recibirás.
¿Cuáles son mis opciones de tratamiento?
Las opciones de tratamiento dependerán del grado y la etapa del cáncer. Si tienes cáncer de vejiga de grado alto sin invasión muscular, el tratamiento suele consistir en la resección transuretral del tumor de la vejiga, seguido de un tratamiento intravesical con quimioterapia o inmunoterapia, como inmunoterapia con el bacilo de Calmette y Guérin. Si tienes un carcinoma invasivo, como cáncer de invasión muscular, el tratamiento generalmente incluye quimioterapia combinada con cisplatino, seguida de la extirpación de la vejiga o radiación. Cada una de estas opciones incluye consideraciones relacionadas con la calidad de vida y la toxicidad que se deben analizar, por lo que el paciente será responsable de decidir la mejor opción para él. La inmunoterapia adyuvante es un tipo de tratamiento que se administra después de la cirugía para ayudar a mitigar el riesgo de recurrencia del cáncer en el futuro. En general, el tratamiento para los pacientes con cáncer de vejiga en etapa 4 consiste en quimioterapia combinada con cisplatino de primera línea.
¿La cirugía debe realizarse de forma robótica?
En realidad, no es un factor importante. Independientemente de si te sometes a una cirugía abierta o a una cirugía robótica, los resultados serán prácticamente los mismos. Como se trata de una operación importante, sin importar cómo se realice, los pacientes deberán pasar algunos días en el hospital después de la cirugía y necesitarán algunas semanas para recuperarse. Sin embargo, si se opta por un enfoque robótico, se realizarán pequeñas incisiones laparoscópicas y, en general, habrá una menor cantidad de pérdida de sangre y de complicaciones relacionadas con la herida. Si se decide hacer una cirugía abierta, el procedimiento será más rápido, pero puede haber una mayor cantidad de pérdida de sangre. A mis pacientes les recomiendo que elijan el tipo de cirugía con la que se sientan más cómodos.
¿Qué es una neovejiga?
Una neovejiga es un tipo de desviación urinaria que se realiza durante la cirugía para extirpar la vejiga. Al extraer la vejiga, es necesario redirigir el flujo de orina hacia algún lugar. Para ello, tomamos aproximadamente 1 pie (unos 30 cm) de la parte inferior del intestino delgado, el íleon, y lo cortamos para abrirlo y crear una esfera. Luego, lo conectamos a la uretra y a los riñones. La ventaja de esto es que todo el sistema está en el interior del cuerpo. No se requiere ninguna bolsa externa de drenaje para la orina, como en el caso de un procedimiento de conducto ileal. Sin embargo, las neovejigas tienen algunas desventajas. No suelen funcionar a la perfección. Por ejemplo, alrededor del 25 % de los hombres y del 30 % de las mujeres sufrirán algún grado de incontinencia a largo plazo. Aproximadamente el 10 % de los hombres y el 25 % de las mujeres deberán vaciar la neovejiga por catéter. Estas consideraciones son importantes a la hora de decidir entre una neovejiga y un conducto ileal.
¿Qué es un conducto ileal?
Un conducto ileal es una forma de desviación urinaria donde se usa una bolsa externa para drenar la orina. A diferencia de la neovejiga, un sistema completamente interno que consiste en crear una vejiga nueva y conectar los riñones a la uretra, el conducto ileal desvía la orina de manera extracorpórea. De este modo, a la derecha del ombligo tendrás un estoma, como una ostomía, que drenará la orina en una bolsa. Para muchos pacientes, esta es la mejor opción. Es un sistema simple y fácil de usar. No tendrás que levantarte por la noche para ir al baño, ni detenerte mientras estás conduciendo. Además, después de la cirugía, podrás hacer todas las actividades que hacías antes del procedimiento, incluidos el buceo, el paracaidismo, el esquí acuático, el golf, el senderismo y el ciclismo. Muchos pacientes se preguntan cuál es la mejor opción de desviación para ellos. Y, de hecho, todo depende de la persona. En el caso de quienes buscan sencillez, el conducto ileal es la opción correcta.
¿De qué forma afectará el tratamiento a mi calidad de vida?
La calidad de vida es una consideración muy importante a la hora de decidir qué opciones de tratamiento son las mejores para ti. En el caso del cáncer de vejiga sin invasión muscular, se suele indicar un tratamiento intravesical. Sin embargo, este tratamiento tiene efectos secundarios, como sensación de ardor al orinar, cambios en la frecuencia o urgencia urinaria, y sangre en la orina. También implica someterse a cateterismos que pueden ser dolorosos durante las administraciones. En el caso de los pacientes que tienen cáncer de invasión muscular y están tratando de decidir entre hacerse una cistectomía (que es la extirpación completa de la vejiga) o recibir radioterapia, también hay una serie de consideraciones sobre la calidad de vida que deben analizarse.
¿Cuál es la mejor manera de colaborar con mi equipo de atención médica?
Los pacientes que participan en su propio cuidado médico son los más fáciles de atender. Infórmate tanto como puedas y recuerda que todos somos parte del mismo equipo. Si tienes preguntas o inquietudes, siempre consulta a tu equipo médico. Estar informado marca la diferencia. Gracias por tu tiempo. Te deseamos lo mejor.
Diagnóstico de cáncer de vejiga
Cistoscopia femenina
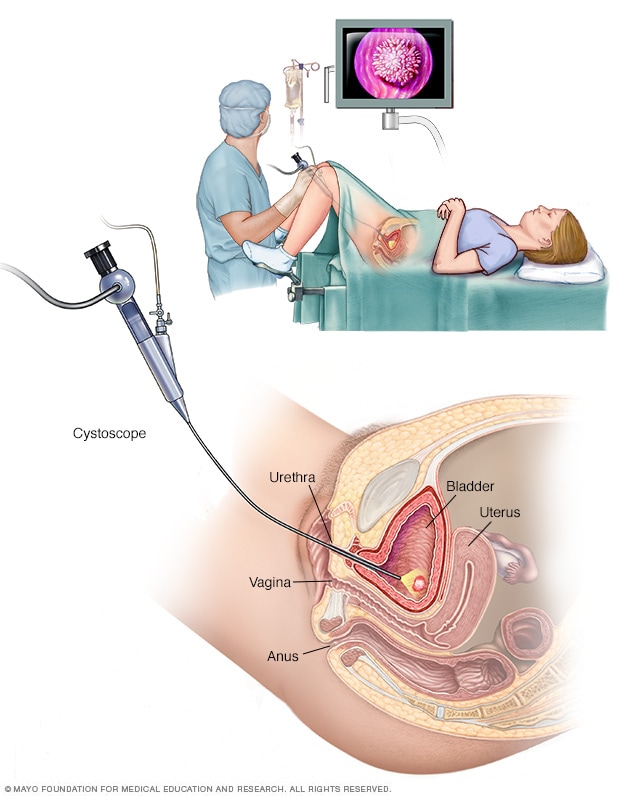
Cistoscopia femenina
La cistoscopia permite al proveedor de atención médica visualizar las vías urinarias inferiores y buscar problemas, como cálculos en la vejiga. Los instrumentos quirúrgicos pueden introducirse por el cistoscopio para tratar determinadas afecciones de las vías urinarias.
Cistoscopia masculina
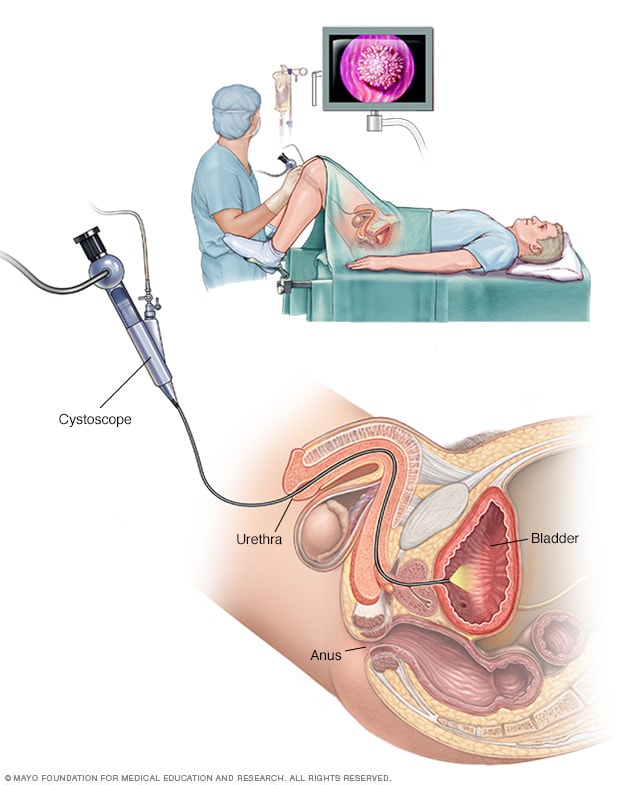
Cistoscopia masculina
La cistoscopia permite que el proveedor de atención médica visualice las vías urinarias inferiores y busque problemas en la uretra y la vejiga. Los instrumentos quirúrgicos pueden introducirse por el cistoscopio para tratar determinadas afecciones de las vías urinarias.
Las pruebas y los procedimientos utilizados para diagnosticar el cáncer de vejiga incluyen lo siguiente:
- Usar un microscopio para examinar el interior de la vejiga (cistoscopia). Para realizar la cistoscopia, el médico inserta un tubo pequeño y estrecho (cistoscopio) a través de la uretra. El cistoscopio tiene una lente que permite al médico ver el interior de la uretra y la vejiga, y examinar estas estructuras en busca de signos de enfermedad. La cistoscopia puede hacerse en el consultorio del médico o en el hospital.
- Extracción de una muestra de tejido para analizarla (biopsia). Durante la cistoscopia, el médico puede insertar un instrumento especial a través del endoscopio y dentro de la vejiga para recoger una muestra de células (biopsia) para analizarla. A veces, este procedimiento se denomina resección transuretral de tumor de vejiga. La resección transuretral de un tumor de vejiga también se puede utilizar para tratar el cáncer de vejiga.
- Examinar una muestra de orina (citología de orina). Se analiza una muestra de orina en un microscopio para determinar si hay células cancerosas en un procedimiento llamado citología de orina.
-
Pruebas por imágenes. Las pruebas por imágenes, como el urograma de tomografía computarizada o el pielograma retrógrado, permiten que el médico examine las estructuras de las vías urinarias.
Durante un urograma por tomografía computarizada, se inyecta una sustancia de contraste en una vena de la mano que finalmente fluye hacia los riñones, los uréteres y la vejiga. Las imágenes de rayos X tomadas durante el examen proporcionan una vista detallada de las vías urinarias y ayudan a que el médico identifique cualquier área que pueda ser cancerosa.
El pielograma retrógrado es un examen de rayos X utilizado para obtener una visión detallada de las vías urinarias superiores. Durante esta prueba, el médico inserta un tubo fino (catéter) a través de la uretra y hasta la vejiga para inyectar una sustancia de contraste en los uréteres. Luego, el tinte fluye hacia los riñones mientras se capturan imágenes radiográficas.
Para determinar la magnitud del cáncer
Después de confirmar que tienes cáncer de vejiga, es posible que el médico te recomiende otras pruebas para determinar si el cáncer se diseminó a los ganglios linfáticos o a otras zonas del cuerpo.
Entre las pruebas, se pueden incluir las siguientes:
- Tomografía computarizada
- Imágenes por resonancia magnética
- Tomografía por emisión de positrones (PET, por sus siglas en inglés)
- Gammagrafía ósea
- Rayos X del tórax
El médico usa la información de estos procedimientos para definir el estadio del cáncer. Los estadios del cáncer de vejiga se indican con números romanos que van del 0 al IV. Los estadios más bajos indican un cáncer que se limita a las capas internas de la vejiga y que no ha crecido hasta afectar la pared muscular de la vejiga. El estadio más alto, el IV, indica que el cáncer se diseminó a los ganglios linfáticos u órganos en zonas distantes del cuerpo
Grado de cáncer de vejiga
Los cánceres de la vejiga se clasifican en función de cómo aparecen las células cancerosas cuando se observan a través de un microscopio. Esto se conoce como el grado, y tu médico podría describir al cáncer de vejiga como de bajo o alto grado:
- Cáncer de vejiga de bajo grado. Este tipo de cáncer tiene células que, en apariencia y organización, son más similares a las células normales (bien diferenciadas). Un tumor de bajo grado suele crecer más lentamente y es menos probable que invada la pared muscular de la vejiga que un tumor de alto grado.
- Cáncer de vejiga de alto grado. Este tipo de cáncer tiene células de aspecto anormal y que no se parecen en nada a los tejidos de apariencia normal (poco diferenciadas). Un tumor de alto grado tiende a crecer de forma más agresiva que un tumor de bajo grado y puede ser más probable que se extienda a la pared muscular de la vejiga y a otros tejidos y órganos.
Más información
Tratamiento
Las opciones de tratamiento para el cáncer de vejiga dependen de varios factores que se tienen en cuenta, como el tipo de cáncer, el grado del cáncer y el estadio del cáncer, además de tu salud general y tus preferencias de tratamiento.
El tratamiento del cáncer de vejiga puede incluir lo siguiente:
- Cirugía, para extirpar las células cancerosas
- Quimioterapia en la vejiga (quimioterapia intravesical), para tratar los cánceres que están confinados al revestimiento de la vejiga pero que tienen un alto riesgo de recurrencia o progresión a un estadio más avanzado
- Quimioterapia para el cuerpo entero (quimioterapia sistémica), para aumentar las probabilidades de curación en una persona que se somete a una cirugía para extirpar la vejiga, o como tratamiento primario cuando la cirugía no es una opción
- Radioterapia, para destruir las células cancerosas, generalmente como tratamiento primario cuando la cirugía no es una opción o no es la opción deseada
- Inmunoterapia, para activar el sistema inmunitario del cuerpo para combatir las células cancerosas, ya sea en la vejiga o en todo el cuerpo
- Terapia dirigida, para tratar el cáncer avanzado cuando otros tratamientos no han ayudado
Tu médico y los miembros de tu equipo de atención médica pueden recomendar una combinación de enfoques de tratamiento.
Cirugía para cáncer de vejiga
Conducto ileal
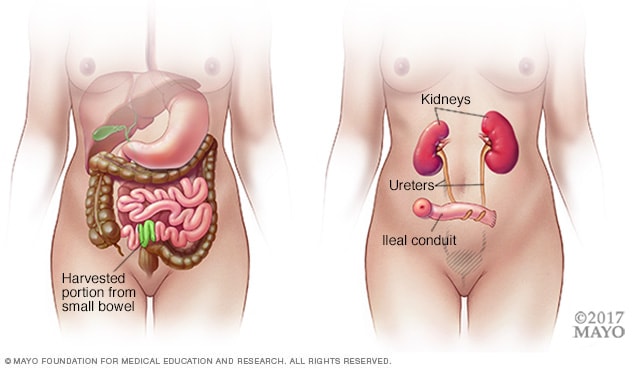
Conducto ileal
Durante un procedimiento de conducto ileal, un cirujano crea un nuevo tubo a partir de un trozo de intestino que permite que los riñones drenen y que la orina se elimine del cuerpo a través de una pequeña abertura llamada estoma.
Reconstrucción de neovejiga
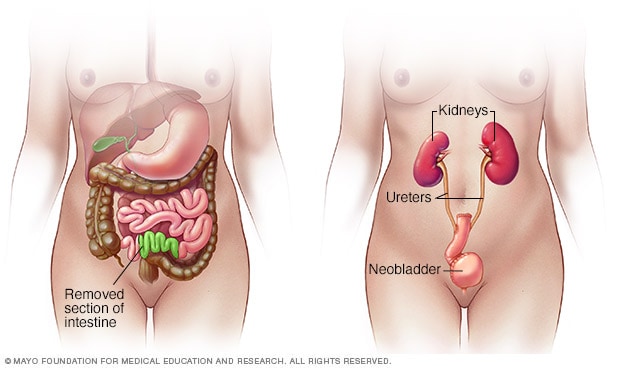
Reconstrucción de neovejiga
Durante la cirugía de neovejiga, el cirujano extrae la vejiga existente y forma una bolsa interna con una parte del intestino. Esta bolsa, que se denomina neovejiga, almacena la orina.
Los enfoques de cirugía de cáncer de vejiga pueden incluir lo siguiente:
-
Resección transuretral de tumor de vejiga. La resección transuretral de tumor de vejiga es un procedimiento para diagnosticar el cáncer de vejiga y eliminar los cánceres presentes en las capas internas de la vejiga, que aún no son cánceres invasivos para los músculos. Durante el procedimiento, el cirujano pasa una guía de cable eléctrico a través de un cistoscopio para ver la vejiga por dentro. La corriente eléctrica en el cable se utiliza para cortar o quemar el cáncer. Alternativamente, se puede usar un láser de gran energía.
Debido a que los médicos realizan el procedimiento a través de la uretra, no tendrás ningún corte (incisión) en el abdomen.
Como parte del procedimiento de resección transuretral de tumor de vejiga, el médico puede recomendar una inyección única de medicamentos para matar el cáncer (quimioterapia) en la vejiga que busca destruir toda célula cancerosa restante y prevenir su reaparición. Los medicamentos permanecen en la vejiga durante un período de tiempo y luego se drenan.
-
Cistectomía. La cistectomía es una cirugía para extirpar toda o parte de la vejiga. Durante una cistectomía parcial, el cirujano retira únicamente la porción de la vejiga que contiene un solo tumor canceroso.
Una cistectomía radical es una operación para extirpar toda la vejiga y los ganglios linfáticos circundantes. En los hombres, la cistectomía radical generalmente consiste en extirpar la próstata y las vesículas seminales. En las mujeres, la cistectomía radical puede implicar la extirpación del útero, de los ovarios y de parte de la vagina.
La cistectomía radical puede realizarse a través de una incisión en la parte inferior del abdomen o con múltiples incisiones pequeñas mediante cirugía robótica. Durante la cirugía robótica, el cirujano se sienta en una consola cercana y utiliza controles manuales para mover con precisión los instrumentos quirúrgicos robóticos.
- Reconstrucción de neovejiga. Después de una cistectomía radical, el cirujano debe crear una nueva forma para que la orina salga del cuerpo (desviación urinaria). Una opción para la desviación urinaria es la reconstrucción de la neovejiga. El cirujano crea un reservorio en forma de esfera a partir de un pedazo de tu intestino. Este reservorio, a menudo llamado neovejiga, se encuentra dentro de tu cuerpo y está adherido a la uretra. La neovejiga permite a la mayoría de las personas orinar normalmente. Una pequeña cantidad de personas tiene dificultades para vaciar la neovejiga y puede necesitar un catéter periódicamente para drenar toda la orina.
- Conducto ileal. Para este tipo de desviación urinaria, el cirujano crea un tubo (conducto ileal) utilizando un trozo de tu intestino. El tubo va desde los uréteres, que drenan los riñones, hasta el exterior del cuerpo, donde la orina se vacía en una bolsa (bolsa de urostomía) que se ubica en el abdomen.
- Reservorio urinario continente. Durante este tipo de procedimiento de desviación urinaria, el cirujano utiliza una sección del intestino para crear una pequeña bolsa (reservorio), que se encuentra dentro de tu cuerpo, para contener la orina. Se drena la orina del reservorio con un catéter a través de una abertura en el abdomen varias veces al día.
Quimioterapia
La quimioterapia utiliza medicamentos para destruir las células cancerosas. En el tratamiento de quimioterapia para el cáncer de vejiga, suelen usarse de forma combinada dos o más fármacos de quimioterapia.
Se pueden administrar fármacos de quimioterapia:
- A través de una vena (por vía intravenosa). La quimioterapia intravenosa se usa con frecuencia antes de la cirugía de extirpación de la vejiga para aumentar las posibilidades de curar el cáncer. La quimioterapia también puede usarse para destruir las células cancerosas que puedan quedar después de la cirugía. En ciertas situaciones, la quimioterapia puede combinarse con la radioterapia.
- Directamente en la vejiga (terapia intravesical). Durante la quimioterapia intravesical, se pasa un tubo a través de la uretra directamente a la vejiga. La quimioterapia se coloca en la vejiga durante un período determinado antes de drenarla. Se puede usar como tratamiento principal para el cáncer de vejiga superficial, donde las células cancerosas afectan solo el revestimiento de la vejiga y no el tejido muscular más profundo.
Radioterapia
La radioterapia utiliza haces de energía poderosa, como rayos X y protones, para destruir las células cancerosas. Generalmente, la radioterapia para el cáncer de vejiga la realiza una máquina que se mueve alrededor del cuerpo y dirige los haces de energía a puntos precisos.
La radioterapia a veces se combina con la quimioterapia para tratar el cáncer de vejiga en ciertas situaciones, por ejemplo, cuando la cirugía no es una opción o no se desea.
Inmunoterapia
La inmunoterapia es un tratamiento con medicamentos que ayuda al sistema inmunitario a combatir el cáncer.
Se puede administrar la inmunoterapia:
- Directamente en la vejiga (terapia intravesical). La inmunoterapia intravesical se puede recomendar después de la resección transuretral de un tumor de vejiga cuando el cáncer de vejiga es pequeño y no ha crecido en las capas musculares más profundas de la vejiga. En este tratamiento se utiliza el bacilo Calmette-Guerin (BCG), que se desarrolló como una vacuna utilizada para proteger contra la tuberculosis. El BCG provoca una reacción del sistema inmunitario que dirige las células que combaten los gérmenes a la vejiga.
- A través de una vena (por vía intravenosa). La inmunoterapia se puede administrar por vía intravenosa cuando el cáncer de vejiga es avanzado o reaparece después del tratamiento inicial. Existen varios medicamentos para la inmunoterapia. Estos medicamentos ayudan a tu sistema inmunitario a identificar y combatir las células cancerosas.
Terapia dirigida
Los medicamentos de la terapia dirigida se centran en debilidades específicas presentes en las células cancerosas. Al atacar estas debilidades, los tratamientos farmacológicos dirigidos pueden causar la muerte de las células cancerosas. Las células cancerosas pueden ser analizadas para ver si la terapia dirigida puede ser eficaz.
La terapia dirigida puede ser una opción para tratar el cáncer de vejiga avanzado cuando otros tratamientos no han funcionado.
Preservación de la vejiga
En ciertas situaciones, las personas con cáncer de vejiga de invasión muscular que no desean someterse a una cirugía para extirpar la vejiga pueden considerar la posibilidad de probar una combinación de tratamientos. Conocido como terapia de trimodalidad, este enfoque combina resección transuretral de tumor de vejiga, quimioterapia y radioterapia.
Primero, el cirujano realiza un procedimiento de resección transuretral de tumor de vejiga para extirpar la mayor cantidad posible de cáncer de la vejiga, preservando la función de la misma. Después de la resección transuretral de tumor de vejiga, te sometes a un régimen de quimioterapia junto con radioterapia.
Si, después de probar la terapia de trimodalidad, no desaparece todo el cáncer o si tienes una recurrencia del cáncer invasivo muscular, tu médico puede recomendar una cistectomía radical.
Después del tratamiento para cáncer de vejiga
El cáncer de vejiga puede reaparecer, incluso después de un tratamiento exitoso. Debido a esto, las personas con cáncer de vejiga necesitan pruebas de seguimiento durante años después de un tratamiento exitoso. Qué pruebas tendrás que hacerte y con qué frecuencia dependerá del tipo de cáncer de vejiga y del tratamiento, entre otros factores.
En general, los médicos recomiendan una prueba para examinar el interior de la uretra y la vejiga (cistoscopia) cada tres a seis meses durante los primeros años después del tratamiento del cáncer de vejiga. Después de algunos años de vigilancia sin detectar la recurrencia del cáncer, es posible que necesites un examen de cistoscopia solo una vez al año. Puede que el médico también te recomiende hacer otras pruebas a intervalos regulares.
Es posible que las personas con casos de cáncer agresivo sean sometidas a análisis con mayor frecuencia. Aquellos con tipos de cáncer menos agresivos pueden someterse a análisis con menor frecuencia.
Video relacionado
Más información
Estudios clínicos
Explora los estudios de Mayo Clinic que ensayan nuevos tratamientos, intervenciones y pruebas para prevenir, detectar, tratar o controlar esta afección.
Estrategias de afrontamiento y apoyo
Si permanentemente te preocupa que el cáncer de vejiga reaparezca, terminarás sintiendo que tienes poco control sobre tu futuro. Pero mientras no haya manera de asegurarse de que el cáncer de vejiga no reaparecerá, puedes tomar algunas medidas para controlar el estrés.
Con el tiempo descubrirás qué es lo que funciona para ti, pero hasta ese momento, puedes hacer lo siguiente:
- Consigue un calendario de pruebas de seguimiento y ve a cada cita. Cuando termines el tratamiento para el cáncer de vejiga, pídele a tu médico que cree un cronograma personalizado de las pruebas de seguimiento. Antes de cada cistoscopia de seguimiento, seguramente sentirás cierta ansiedad. Puedes sentir temor de que el cáncer haya reaparecido o preocuparte por lo molesto del examen. No dejes que esto te impida ir a la cita. Por el contrario, piensa en formas de enfrentar tu preocupación. Anota tus pensamientos en un diario, habla con un amigo o practica técnicas de relajación, como la meditación.
- Cuídate a fin de estar listo para combatir el cáncer, si es que regresa. Cuídate y ajusta tu dieta asegurándote de que incluya abundantes frutas, verduras y cereales integrales. Realiza ejercicio la mayoría de los días de la semana durante, por lo menos, treinta minutos. Duerme lo suficiente para despertar sintiéndote renovado.
- Habla con otras personas que hayan sobrevivido al cáncer de vejiga. Conéctate con personas que hayan sobrevivido al cáncer de vejiga y que tengan los mismos temores que tú. Ponte en contacto con tu delegación local de la American Cancer Society (Sociedad Estadounidense contra el Cáncer) para saber si hay grupos de apoyo para el cáncer en tu zona.
Preparación para la consulta
Comienza por visitar a tu médico de cabecera si tienes algún signo o síntoma que te preocupe, como sangre en la orina. El médico puede sugerirte análisis y procedimientos para investigar tus signos y síntomas.
Si el médico sospecha que puedes tener cáncer de vejiga, puede remitirte a un médico que se especializa en el tratamiento de enfermedades y afecciones de las vías urinarias (urólogo). En algunos casos, es posible que te remitan a otros especialistas; por ejemplo, los médicos que tratan el cáncer (oncólogos).
Generalmente, hay mucha información para analizar, por lo tanto, es una buena idea estar bien preparado. La siguiente información te ayudará a prepararte y a saber qué esperar del médico.
Qué puedes hacer
- Ten en cuenta cualquier restricción previa a la cita. Cuando programes la cita, pregunta si hay algo que debas hacer con anticipación, como restringir tu dieta.
- Anota los síntomas que tengas, incluidos aquellos que quizás no parezcan relacionados con el motivo de la cita.
- Anota información personal clave, como episodios de estrés importantes o cambios recientes en tu vida.
- Haz una lista de todos los medicamentos, las vitaminas o los suplementos que estés tomando junto con las dosis.
- Considera pedirle a un familiar o a un amigo de confianza que te acompañe. A veces es difícil recordar toda la información proporcionada durante una cita. La persona que te acompañe podría recordar algún detalle que tú hayas pasado por alto u olvidado.
- Escribe preguntas para hacerle al médico.
Preparar una lista de preguntas puede ayudarte a aprovechar al máximo el tiempo con el médico. En el caso del cáncer de vejiga, algunas preguntas básicas que se deben hacer incluyen:
- ¿Tengo cáncer de vejiga o mis síntomas podrían ser causados por otra afección?
- ¿En qué estadio está el cáncer que tengo?
- ¿Necesitaré hacerme algún examen adicional?
- ¿Cuáles son mis opciones de tratamiento?
- ¿Existen tratamientos para curar mi cáncer de vejiga?
- ¿Cuáles son los posibles riesgos de cada tratamiento?
- ¿Hay algún tratamiento que crea que es el mejor para mí?
- ¿Debería consultar a un especialista? ¿Cuánto costará? ¿Lo cubrirá mi seguro?
- ¿Existe alguna alternativa genérica al medicamento que me receta?
- ¿Hay algún folleto u otro material impreso que pueda llevarme? ¿Qué sitios web me recomienda?
- ¿Qué determinará si debo programar una visita de seguimiento?
Además de las preguntas que preparaste para hacerle al médico, no dudes en hacer cualquier otra pregunta que se te ocurra.
Qué esperar de tu doctor
Es probable que el doctor te haga varias preguntas. Estar preparado para responderlas puede darte más tiempo para hablar sobre otros temas. Quizás tu doctor te pregunte:
- ¿Cuándo comenzaste a experimentar síntomas?
- Tus síntomas, ¿han sido continuos u ocasionales?
- ¿Cómo son de serios tus síntomas?
- ¿Hay algo que parezca mejorarlos?
- ¿Hay algo que parezca empeorarlos?