Nov. 23, 2023
Although rare, arteriovenous malformations (AVMs) in the brain can have devastating consequences. AVMs vary greatly in terms of risks posed to patients, and there are several treatment options — further complicating care for patients with this intricate vascular pathology.
"Successful AVM management requires a deep dive into all these issues," says Bernard R. Bendok, M.D., chair of Neurosurgery at Mayo Clinic in Phoenix/Scottsdale, Arizona. "There are multiple techniques for managing AVMs, and it's ideal to be seen at a center that excels in all of them."
Mayo Clinic has a large group of neurosurgeons with experience in diverse AVM treatments.
"This disease has so many variables that no single strategy would work for all patients."
"Some of us have expertise in radiosurgery. Others have experience in surgery and embolization, or embolization alone," says Giuseppe Lanzino, M.D., a neurosurgeon at Mayo Clinic in Rochester, Minnesota. "We can be comprehensive in our approach but use our individual strengths in various techniques to the patient's advantage."
Other treatment approaches include stereotactic radiosurgery, awake surgery and watchful waiting.
"If the patient is asymptomatic, sometimes it is better to leave the lesion and monitor it. But if treatment is needed, we discuss which modality or modalities would be best," says Rabih G. Tawk, M.D., a neurosurgeon at Mayo Clinic in Jacksonville, Florida. "The goal is to solve that particular patient's problem, with minimal risk."
Assessing an AVM's risks
The most potent factor influencing an AVMs risk is prior hemorrhage. But signs of AVM bleeding can be subtle. "Susceptibility-weighted imaging might be required to see the hemorrhage," Dr. Bendok says.
An AVM's size and location also affect risk. In general, small AVMs and AVMs located deep in the brain are likelier to bleed. A brain aneurysm, which is found in about 20% of people with an AVM, also increases bleeding risk.
Full understanding of an AVM's potential danger requires detailed imaging. "Mayo Clinic neuroradiologists devote their careers to evaluating brain conditions. This deep experience results in more accurate imaging and interpretation," says Harry Cloft, M.D., Ph.D., a neuroradiologist at Mayo Clinic's campus in Minnesota. "We are continuously updating our imaging equipment and techniques, developing and incorporating the latest advancements in imaging."
AVM imaging starts with cerebral angiography. "It provides the most detailed evaluation," Dr. Cloft says. "In some cases of small AVM, cerebral angiography is the only test that can conclusively make the diagnosis. In all cases, it gives anatomic information that allows for treatment planning."
To obtain clear views of cerebral anatomy and real-time blood flow, Mayo Clinic uses 3D models produced from MR angiography. "AVMs are three-dimensional. It's important to go beyond 2D views of a 3D problem," Dr. Bendok says.
 عرض ثلاثي الأبعاد
عرض ثلاثي الأبعاد
على اليسار، توفر تقنية الواقع المعزز الفلورية عرضًا ثلاثي الأبعاد بالألوان لتمدد الأوعية الدموية (المشار إليها بالسهم الأصفر). وعلى اليمين، توفر التقنية الفلورية عرضًا ثلاثي الأبعاد لتدفق الدم أثناء التدخل الجراحي.
Holography and augmented reality visualization provide additional information. "This combined imaging gives a better understanding of the flow dynamics to the AVM and the draining vessels, and how they intertwine with the underlying anatomy and functioning of the brain," says Chandan Krishna, M.D., a neurosurgeon at Mayo Clinic's campus in Arizona. "We can also see the normal vein tracks around the AVM, and then superimpose a functional MRI to plan a safe and effective surgical corridor. The more information we have, the safer the surgery becomes."
Matching treatment to patient needs
Small AVMs can sometimes be treated with glue embolization to avoid surgery. Endovascular embolization also can be used to stem blood flow before follow-up surgery. "If we know the AVM is going to bleed heavily during surgery, we do embolization first to cut the blood supply and make the surgery safer," Dr. Lanzino says.
"AVMs are three-dimensional. It's important to go beyond 2D views of a 3D problem."
Gamma knife and proton beam radiosurgery can successfully treat AVMs that are less than 2 to 3 centimeters in diameter. Patients are closely monitored for recurrence of bleeding, as it may take a few years for the AVM to resolve. Radiosurgery also can be used to treat AVMs considered inoperable, including AVMs located in the brainstem.
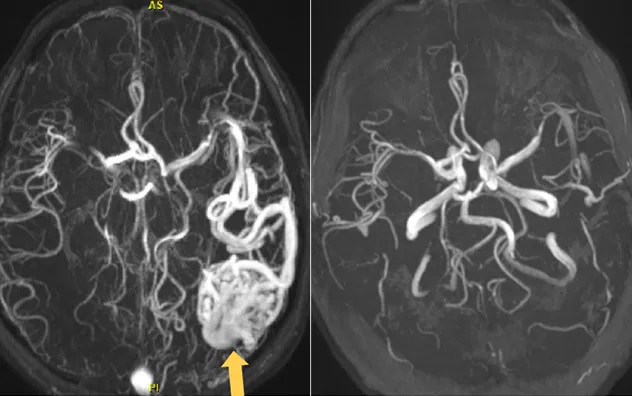 الجراحة الإشعاعية المرحلية
الجراحة الإشعاعية المرحلية
على اليسار، يُظهر تصوير الأوعية بالرنين المغناطيسي تشوهًا شريانيًا وريديًا (يُشار إليه بالسهم الأصفر). على اليمين، يُظهر تصوير الأوعية بالرنين المغناطيسي اختفاء مشكلة التشوه بعد الجراحة الإشعاعية المرحلية.
For larger AVMs, Mayo Clinic uses staged radiosurgery. "Dividing the AVM into two or three pieces and treating each component three months apart has a 50% chance of obliterating the AVM," Dr. Bendok says.
Stereotactic radiosurgery is sometimes followed by surgical resection. "An AVM treated with radiosurgery might still have a small portion that doesn't respond, even after five years. But then it's relatively easy to do surgery on that smaller AVM," Dr. Lanzino says.
For patients with AVM-associated aneurysms, Mayo Clinic takes advantage of the latest treatment devices. Stents with anti-thrombotic coatings reduce the risk of occlusion in parent arteries. Intrasaccular flow disruption devices help overcome the challenges of achieving occlusion in selected wide-necked bifurcation aneurysms.
"These advances are chipping away at the risk of treating aneurysms and offering more less invasive options to the surgical team," Dr. Bendok says.
Defining optimal management
Mayo Clinic participates in an international, multicenter study and patient registry aimed at offering patients the best possible management of AVMs. The Treatment of Brain AVMs Study (TOBAS) encompasses clinical trials testing whether preventive treatments and pre-embolization benefit patients.
As described in the April 2023 issue of the Journal of Neurosurgery, surgical management of AVMs in the TOBAS registry was curative in 88% of patients. The registry included individuals with ruptured and unruptured AVMs.
As research continues, Mayo Clinic remains committed to personalized treatment for AVMs. "This disease has so many variables that no single strategy would work for all patients," Dr. Tawk says. "It's important to have all these strategies available and to be able to perform them in a very advanced way, to ensure that the patient is receiving the best possible care."
For more information
Darsaut TE, et al. Surgical treatment of brain arteriovenous malformations: Clinical outcomes of patients included in the registry of a pragmatic randomized trial. Journal of Neurosurgery. 2023;138:891.
Mayo Clinic. Treatment of Brain AVMs Study (TOBAS). ClinicalTrials.gov.
Refer a patient to Mayo Clinic.