Oct. 04, 2023
Nonalcoholic fatty liver disease (NAFLD) has a new name. It's now known as metabolic dysfunction-associated steatotic liver disease (MASLD). With the updated terminology, the condition of steatotic liver disease is now labeled and diagnosed using affirming language, eliminating any stigmatizing terms associated with alcohol consumption or the use of the word "fatty."
 ترسّبات الدهون في الكبد الدهني
ترسّبات الدهون في الكبد الدهني
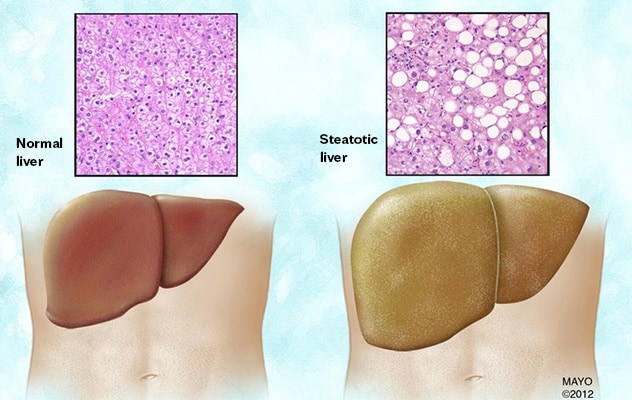
تتضح ترسّبات الدهون في الكبد الدهني مقارنةً بالكبد الطبيعي على المستوى الخلوي.
MASLD occurs when fat deposits in the liver damage liver cells. This can lead to liver inflammation, scarring, cirrhosis and possibly the need for a liver transplant. Other systemic problems may follow, including cardiovascular complications.
MASLD is the leading cause of liver disease among children today. It affects up to 38% of children with obesity in the United States, although not all children with MASLD have obesity. Of note, the prevalence of MASLD has increased 2.7 times since the late 1980s, according to a 2017 study in the Journal of Pediatric Gastroenterology and Nutrition. An analysis of the global prevalence of MASLD in adolescents in 2019 was 4.7%, as cited in a study in Hepatology.
According to Sara Hassan, M.D., a pediatric transplant hepatologist and gastroenterologist at Mayo Clinic in Rochester, Minnesota, MASLD is the primary cause of pediatric liver disease in the children she sees in her practice at Mayo Clinic Children's Center. She describes the urgency of the issue: "We have to address it. We have to do something now."
"Diagnosis and treatment at the Mayo Clinic Steatotic Liver Clinic take a two-pronged approach," says Samar H. Ibrahim, M.B., Ch.B., a pediatric transplant hepatologist and gastroenterologist at Mayo Clinic in Minnesota and co-director of the steatotic liver clinic along with Dr. Hassan. First, patients undergo screening to rule out other causes for elevated liver enzymes. Then, once a diagnosis has been made, patients receive counseling about how to manage MASLD. This may include consults with a dietitian or referral to a weight management center. Follow-up takes place every 3 to 6 months and includes a review of liver enzyme levels and other biometric markers. If liver enzymes remain high, patients may undergo additional testing and more-intensive monitoring.
Screening for MASLD includes assessment of liver enzymes, particularly alanine aminotransferase. However, a diagnosis of MASLD cannot be established until other causes of elevated liver enzymes have been eliminated, which may include metabolic disorders, nutritional deficiencies, genetic disorders such as Wilson's disease, certain medications and infections such as viral hepatitis.
Other tools that may be useful in diagnosis include ultrasound, liver biopsy and magnetic resonance imaging with magnetic resonance elastography. A noninvasive ultrasound-based tool is gaining interest and widespread use among pediatric hepatologists to determine how much fat is in the liver. It also is used to detect the presence and severity of fibrosis. A subset of patients with persistent elevation of liver enzymes may need a liver biopsy to assess the severity of nonalcoholic steatohepatitis as well as exclude other treatable liver disease.
Pediatricians at Mayo Clinic Children's Center work closely with a multidisciplinary team to provide integrated care for children with MASLD. "The Steatotic Liver Clinic is an integral part of the obesity task force, and we work closely with the bariatric surgery team as well," explains Dr. Hassan.
Each member of the multidisciplinary team provides unique insight and support for patients with MASLD, such as obesity gene testing through the weight management clinic. A very small subset of patients with early-onset obesity and MASLD might have rare monogenic causes of obesity (for example, mutations in the melanocortin 4 receptor gene or congenital leptin deficiency). These conditions have specific treatments and are important to identify early in life. "However, a larger proportion of patients have genetic variants — for example, PNPLA3 — that do not cause but predispose to obesity and MASLD, which manifest in a permissive environment of sedentary lifestyle and a diet high in fat, fructose and cholesterol," explains Dr. Ibrahim.
Patients with MASLD often present with several comorbidities that may complicate both diagnosis and treatment. In addition to obesity, patients may have hypertension, obstructive sleep apnea, polycystic ovarian syndrome, kidney disease or orthopedic issues such as knee pain or referred hip pain related to excess weight.
MASLD can be reversed through weight loss by implementing dietary changes and regular exercise. While minimal reductions in weight loss (3% to 5% of body weight) can significantly impact fat deposits in the liver, it can be difficult for patients with MASLD to implement lifestyle changes for several reasons.
"It's really easy to just say, 'You need to lose weight.' But that's not going to get us anywhere in treatment," explains Dr. Hassan.
Patient education about healthy diet and exercise is often complicated by limiting factors, such as deconditioning or pain due to excess weight.
Other patients cannot access safe playgrounds, or they live in single-parent households with limited time for outdoor exercise. Others have emotional or psychological issues that complicate their relationship with food.
Dr. Hassan helps her patients identify incremental, actionable steps to which they are more likely to adhere. For example, she often recommends that her adolescent patients choose a 20-minute playlist of "energy music" they can listen to while walking the dog or doing yardwork.
Dr. Hassan also prefers to take the emphasis off exercising to lose weight, which can be a difficult subject for children and teenagers. She says, "While we do encourage 1 to 2 pounds (0.5 to 1 kilogram) of weight loss a month, we focus more on a comprehensive approach to promote a healthier lifestyle with dietary changes and exercise."
It also is important to include parents and other family members in the treatment plan, which may include substantial shifts to the family diet. However, Dr. Hassan emphasizes that she avoids counseling her patients to eliminate or avoid foods altogether. Instead, she encourages her patients to think about quantity and frequency.
"How we talk about food and weight is really important. If we only emphasize weight loss, we risk creating eating disorders," Dr. Hassan continues. "It's a very fine line to walk."
There are no Food and Drug Administration-approved medical therapies for MASLD to date. Ongoing research to find safe and effective therapeutic agents in Dr. Ibrahim's laboratory have focused on alleviating the inflammatory response and the cellular stress produced by circulating toxic lipids in patients with MASLD. Preclinical experimental drug studies in mouse models of MASLD have shown success in attenuating liver inflammation and the development of liver fibrosis; however, these agents require extensive validation before early clinical trials are considered.
For more information
Vos MB, et al. NASPGHAN clinical practice guideline for the diagnosis and treatment of nonalcoholic fatty liver disease in children. Journal of Pediatric Gastroenterology and Nutrition. 2017;64:319.
Hartmann P, et al. Global and national prevalence of nonalcoholic fatty liver disease in adolescents: An analysis of the global burden of disease study 2019. Hepatology. In Press.
Mayo Clinic Children's Center.