Diagnosis
Your doctor may do a series of tests to determine the cause of your dizziness. During a physical exam, your doctor will likely look for:
- Signs and symptoms of dizziness that are prompted by eye or head movements and then decrease in less than one minute
- Dizziness with specific eye movements that occur when you lie on your back with your head turned to one side and tipped slightly over the edge of the examination bed
- Involuntary movements of your eyes from side to side
- Inability to control your eye movements
If your doctor can't find the cause of your signs and symptoms, he or she may order additional testing, such as:
- Electronystagmography (ENG) or videonystagmography (VNG). The purpose of these tests is to detect abnormal eye movement. ENG (which uses electrodes) or VNG (which uses small cameras) can help determine if dizziness is due to inner ear disease by measuring involuntary eye movements while your head is placed in different positions or your balance organs are stimulated with water or air.
- Magnetic resonance imaging (MRI). This test uses a magnetic field and radio waves to create cross-sectional images of your head and body. Your doctor can use these images to identify and diagnose a range of conditions. MRI may be performed to rule out other possible causes of vertigo.
Treatment
The inner ear and canalith repositioning
The inner ear and canalith repositioning
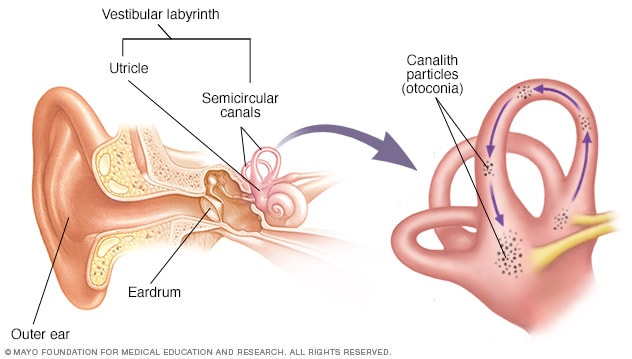
Vertigo is caused by a problem with the nerves and structures in the inner ear that control balance (vestibular labyrinth). Benign paroxysmal positional vertigo (BPPV) occurs when tiny canalith particles (otoconia) break loose and fall into the wrong part of the semicircular canals of the inner ear. The goal of the canalith repositioning procedure is to move the particles from the inner ear to a part of the ear where they won't cause problems (the utricle).
Benign paroxysmal positional vertigo may go away on its own within a few weeks or months. But, to help relieve BPPV sooner, your doctor, audiologist or physical therapist may treat you with a series of movements known as the canalith repositioning procedure.
Canalith repositioning
Performed in your doctor's office, the canalith repositioning procedure consists of several simple and slow maneuvers for positioning your head. The goal is to move particles from the fluid-filled semicircular canals of your inner ear into a tiny baglike open area (vestibule) that houses one of the otolith organs in your ear, where these particles don't cause trouble and are more easily resorbed.
Each position is held for about 30 seconds after any symptoms or abnormal eye movements stop. This procedure usually works after one or two treatments.
Your doctor will likely teach you how to perform the procedure on yourself so that you can do it at home if needed.
Surgical alternative
In rare situations when the canalith repositioning procedure doesn't work, your doctor may recommend a surgical procedure. In this procedure, a bone plug is used to block the portion of your inner ear that's causing dizziness. The plug prevents the semicircular canal in your ear from being able to respond to particle movements or head movements in general. The success rate for canal plugging surgery is about 90%.
Lifestyle and home remedies
If you experience dizziness associated with BPPV, consider these tips:
- Be aware of the possibility of losing your balance, which can lead to falling and serious injury.
- Avoid movements, such as looking up, that bring on the symptoms.
- Sit down immediately when you feel dizzy.
- Use good lighting if you get up at night.
- Walk with a cane for stability if you're at risk of falling.
- Work closely with your doctor to manage your symptoms effectively.
BPPV may recur even after successful therapy. Although there's no cure, the condition can be managed with physical therapy and home treatments.
Preparing for your appointment
Make an appointment with your doctor if you have symptoms common to BPPV. After an initial examination, your doctor may refer you to an ear, nose and throat (ENT) specialist or a doctor who specializes in the brain and nervous system (neurologist).
Here's some information to help you get ready for your appointment.
What you can do
- Write down your symptoms, including when they started and how often they occur.
- Note any recent blows to your head, including even minor accidents or injuries.
- Make a list of your key medical information, including any other conditions for which you're being treated and the names of any medications, vitamins and supplements you're taking.
- Write down questions to ask your doctor. Creating your list of questions can help you make the most of your time with your doctor.
Questions to ask the doctor at the initial appointment include:
- What are the possible causes of my symptoms or condition?
- What tests do you recommend?
- If these tests don't pinpoint the cause of my symptoms, what additional tests might I need?
- Do I need to follow any restrictions while waiting for a diagnosis?
- Should I see a specialist?
Questions to ask if you are referred to a specialist include:
- What treatments are most likely to help me feel better?
- How soon after beginning treatment should my symptoms start to improve?
- If the first treatment doesn't work, what will you recommend next?
- Am I a candidate for surgery? Why or why not?
- What self-care steps can help me manage this condition?
- Do I need to restrict my activities? For how long?
- Am I at risk of this problem recurring?
- I have these other health conditions. How can I manage these conditions together?
- What handouts or websites do you recommend for learning more about BPPV?
What to expect from your doctor
A doctor who sees you for symptoms common to BPPV may ask a number of questions, such as:
- What are your symptoms, and when did you first notice them?
- Do your symptoms come and go? How often?
- How long do your symptoms last?
- Does anything in particular seem to trigger your symptoms, such as certain types of movement or activity?
- Do your symptoms include vision problems?
- Do your symptoms include nausea or vomiting?
- Do your symptoms include headache?
- Have you lost any hearing?
- Are you being treated for any other medical conditions?
Aug. 05, 2022