Overview
The liver
The liver
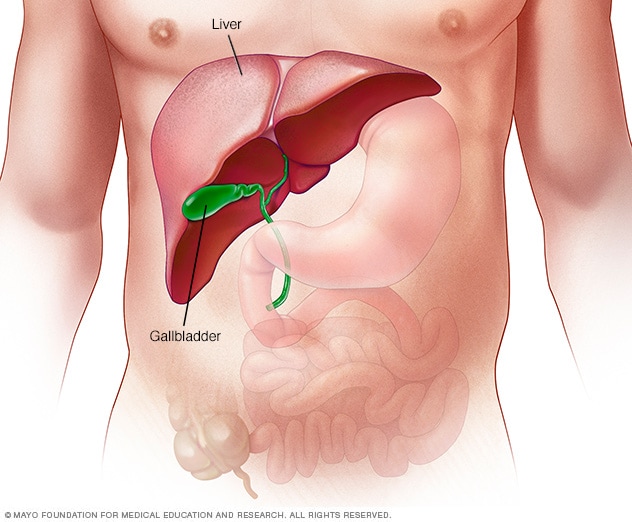
The liver is the largest internal organ. About the size of a football, it's located mainly in the upper right portion of the abdomen, beneath the diaphragm and above the stomach.
Toxic hepatitis is inflammation of the liver in response to toxins. Alcohol, chemicals, medicines or nutritional supplements can cause toxic hepatitis.
Sometimes, toxic hepatitis comes on within hours or days of being in contact with a toxin. Other times, it can take months of regular exposure before symptoms appear.
The symptoms of toxic hepatitis often go away when contact with the toxin stops. But toxic hepatitis can damage the liver, leading to scarring of liver tissue, called cirrhosis. Sometimes toxic hepatitis causes liver failure, which can be life-threatening.
Products & Services
Symptoms
Mild toxic hepatitis might not cause symptoms. It might be found with blood tests. When symptoms of toxic hepatitis occur, they can include:
- Yellowing of the skin, which may be easier to see on white skin. Yellowing of the whites of the eyes. This yellowing is called jaundice.
- Itching.
- Pain in the upper right part of the stomach area.
- Fatigue.
- Loss of appetite.
- Nausea and vomiting.
- Rash.
- Fever.
- Weight loss.
- Dark or tea-colored urine.
When to see a doctor
See a healthcare professional right away if you have symptoms that worry you.
Taking too much of some medicines, such as acetaminophen (Tylenol, others), may lead to liver failure. Get medical care right away for an adult or a child who has taken too much acetaminophen. Symptoms of a possible acetaminophen overdose include:
- Loss of appetite.
- Nausea and vomiting.
- Pain in the upper stomach area.
- Coma.
If you suspect an acetaminophen overdose, immediately call 911 or your local emergency services. In the United States, call a poison control center at 800-222-1222. Do not wait to see symptoms. An acetaminophen overdose can be fatal. But it can be treated soon after the acetaminophen is taken.
Causes
Toxic hepatitis happens when a substance causes swelling, called inflammation, in the liver.
Most of the time, the liver removes and breaks down most chemicals from the bloodstream. Breaking down toxins makes byproducts that can damage the liver. The liver has a great ability to heal itself. But constant contact with toxic substances can cause serious harm. Sometimes the harm can't be fixed.
Causes of toxic hepatitis include:
- Alcohol. Heavy drinking over many years can lead to alcoholic hepatitis. Not all heavy drinkers get alcoholic hepatitis. And some people who drink much less can get the disease. This can lead to liver failure.
- Pain relievers available without a prescription. Pain relievers such as acetaminophen, aspirin, ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve) can damage the liver. Taking them often or with alcohol can cause more damage.
- Prescription medicines. Some medicines linked to liver injury include statin medicines used to treat high cholesterol, the combined medicine amoxicillin-clavulanate (Augmentin), phenytoin (Dilantin, Phenytek), azathioprine (Azasan, Imuran), niacin (Niacor), ketoconazole, certain antivirals and anabolic steroids. There are many others.
- Herbs and supplements. Herbs that can harm the liver include aloe vera, black cohosh, cascara, chaparral, comfrey, kava and ephedra. There are many others. Children can get liver damage if they take large doses of vitamins thinking they're candy.
- Chemicals on the job. Common chemicals that can cause liver damage include the dry cleaning solvent carbon tetrachloride, a substance called vinyl chloride that's used to make plastics, the herbicide paraquat and a group of industrial chemicals called polychlorinated biphenyls.
Risk factors
Factors that might increase the risk of toxic hepatitis include:
- Having liver disease. People with a serious liver condition such as cirrhosis or metabolic dysfunction-associated steatotic liver disease are more likely to react to toxins.
- Having hepatitis. Infection with a hepatitis virus makes the liver more likely to be affected by toxins. Infections include hepatitis B, hepatitis C and infections caused by less common hepatitis viruses.
- Aging. With age, the liver breaks down harmful substances more slowly. So toxins stay in the body longer.
- Sex. Women seem to process, also called metabolize, certain toxins more slowly than men do. So their livers are in contact with higher amounts of harmful substances longer. This increases the risk of toxic hepatitis.
- Having certain gene changes, also called mutations. Inheriting certain gene changes that affect the liver enzymes that break down toxins might increase the risk of toxic hepatitis.
Complications
Typical liver versus liver cirrhosis
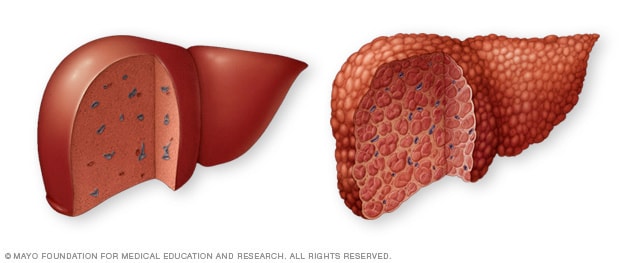
Typical liver versus liver cirrhosis
A typical liver (left) shows no signs of scarring. In cirrhosis (right), scar tissue replaces healthy liver tissue.
The swelling, called inflammation, of toxic hepatitis can lead to liver damage and scarring. Over time, this scarring, called cirrhosis, makes it hard for the liver to do its job.
Toxic hepatitis, even without cirrhosis, can lead to liver failure. The only cure for ongoing liver failure is to replace the liver with a healthy one from a donor, called a liver transplant.
Prevention
Because you can't know how you'll react to a medicine, you can't always prevent toxic hepatitis. But you might cut the risk of liver problems if you:
- Limit medicines. Take medicine only when you must. Instead, look for lifestyle choices for common problems such as high blood pressure, high cholesterol and arthritis pain.
- Take medicines only as directed. Follow the directions exactly for any medicine you take. Don't take more than the dose amount, even if symptoms don't seem to improve. It can be easy to take too much of medicines that wear off before it's time for the next dose.
- Be cautious with herbs and supplements. Natural products can cause harm. Discuss the benefits and risks with a healthcare professional before taking herbs and supplements. The National Institutes of Health has the LiverTox website. It shows medicines and supplements that are linked to liver damage.
- Don't mix alcohol and medicines. If you're taking acetaminophen, don't drink alcohol. Ask a healthcare professional or pharmacist about how alcohol affects other medicines you use.
- Be careful with chemicals. If you work with or use dangerous chemicals, take all measures to protect yourself from them. If you come into contact with a harmful substance, follow the guidelines in your workplace. Or call your local emergency services or a poison control center for help.
- Keep medicines and chemicals away from children. Use childproof containers and keep them out of children's reach.
Aug. 05, 2025