Overview
The liver
The liver
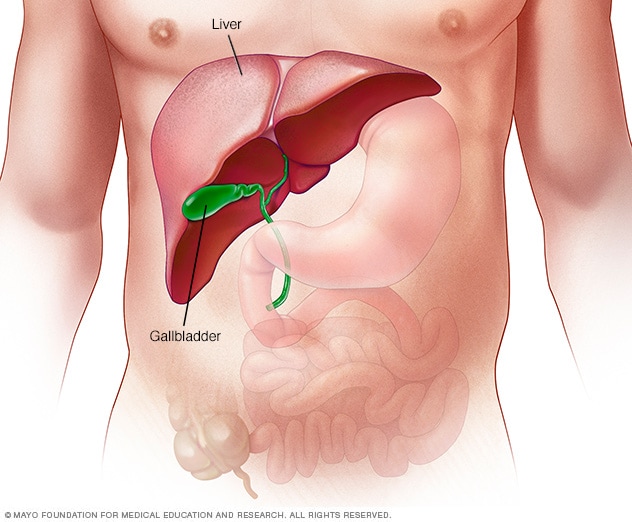
The liver is your largest internal organ. About the size of a football, it's located mainly in the upper right portion of your abdomen, beneath the diaphragm and above your stomach.
Hepatitis C is a viral infection that causes liver swelling, called inflammation. Hepatitis C can lead to serious liver damage. The hepatitis C virus (HCV) spreads through contact with blood that has the virus in it.
Newer antiviral medicines are the treatment of choice for most people with the ongoing, called chronic, hepatitis C infection. These medicines often can cure chronic hepatitis C.
But many people with hepatitis C don't know they have it. That's mainly because symptoms can take decades to appear. So, the U.S. Preventive Services Task Force recommends that all adults ages 18 to 79 years be screened for hepatitis C.
Screening is for everyone, even those who don't have symptoms or known liver disease.
Symptoms
Every long-term hepatitis C infection starts with what's called an acute phase. Acute hepatitis C usually isn't diagnosed because it rarely causes symptoms. When there are symptoms in this phase, they may include jaundice, fatigue, nausea, fever and muscle aches.
Long-term infection with the hepatitis C virus is called chronic hepatitis C. Chronic hepatitis C usually has no symptoms for many years. Symptoms appear only after the virus damages the liver enough to cause them.
Symptoms can include:
- Bleeding easily.
- Bruising easily.
- Fatigue.
- Not wanting to eat.
- Yellowing of the skin, called jaundice. This might show up more in white people. Also, yellowing of the whites of the eyes in white, Black and brown people.
- Dark-colored urine.
- Itchy skin.
- Fluid buildup in the stomach area, called ascites.
- Swelling in the legs.
- Weight loss.
- Confusion, drowsiness and slurred speech, called hepatic encephalopathy.
- Spiderlike blood vessels on the skin, called spider angiomas.
Acute hepatitis C infection doesn't always become chronic. Some people clear the infection from their bodies after the acute phase. This is called spontaneous viral clearance. Antiviral therapy also helps clear acute hepatitis C.
Causes
Hepatitis C infection is caused by the hepatitis C virus (HCV). The infection spreads when blood that has the virus enters the bloodstream of a person who isn't affected.
Around the world, hepatitis C infection exists in several forms, called genotypes. There are seven genotypes and 67 subtypes. The most common hepatitis C genotype in the United States is type 1.
Chronic hepatitis C follows the same course no matter what the genotype of the infecting virus. But treatment can vary depending on viral genotype. However, newer antiviral drugs can treat many genotypes.
Risk factors
Screening for hepatitis C
The U.S. Preventive Services Task Force recommends that all adults ages 18 to 79 years be screened for hepatitis C. Screening is very important for people at high risk of exposure. This includes:
- Anyone who has ever injected, snorted or inhaled an illegal drug.
- Anyone who has atypical liver test results in which the cause wasn't found.
- Babies born from someone who has hepatitis C.
- Pregnant people during the pregnancy.
- Healthcare and emergency workers who have been in contact with blood or been stuck by a needle.
- People with hemophilia who were treated with clotting factors before 1987.
- People who have had long-term hemodialysis.
- People who got donated blood or organ transplants before 1992.
- Sexual partners of anyone diagnosed with hepatitis C infection.
- People with HIV infection.
- Men who have sex with men.
- Sexually active people about to start taking medicine to prevent HIV, called pre-exposure prophylaxis or PrEP.
- Anyone who has been in prison.
Complications
Healthy liver vs. liver cirrhosis
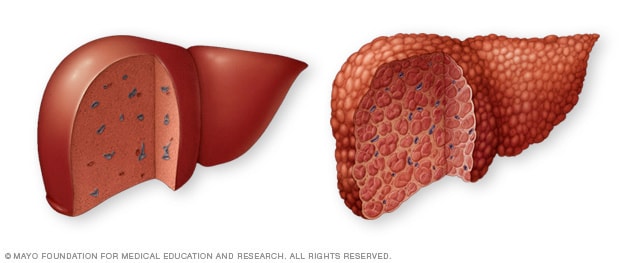
Healthy liver vs. liver cirrhosis
A typical liver, shown on the left, shows no signs of scarring. In cirrhosis, shown on the right, scar tissue replaces typical liver tissue.
Liver cancer
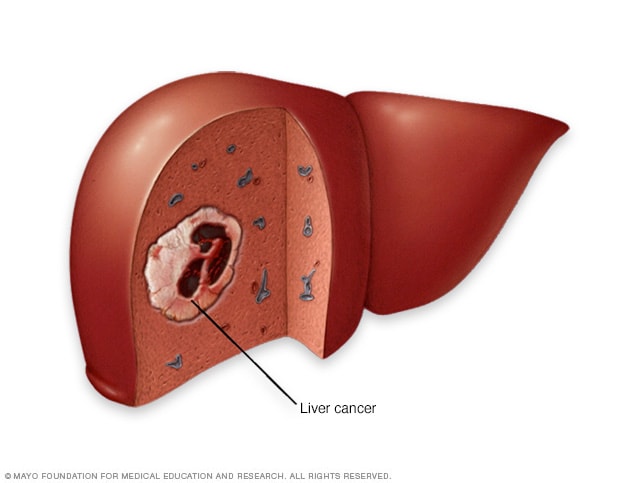
Liver cancer
Liver cancer begins in the cells of the liver. The most common form of liver cancer begins in cells called hepatocytes. This type of cancer is called hepatocellular carcinoma.
Hepatitis C infection that continues over many years can cause serious complications, such as:
- Scarring of the liver, called cirrhosis. Scarring can occur after decades of hepatitis C infection. Liver scarring makes it hard for the liver to work.
- Liver cancer. A small number of people with hepatitis C infection get liver cancer.
- Liver failure. A lot of scarring can cause the liver to stop working.
Prevention
The following might protect from hepatitis C infection:
- Stop using illegal drugs. If you use illegal drugs, seek help.
- Be careful about body piercing and tattooing. For piercing or tattooing, look for a shop that's known to be clean. Ask questions about how the equipment is cleaned. Make sure the employees use sterile needles. If employees won't answer questions, look for another shop.
- Practice safer sex. Don't have sex without protection with any partner whose health status you don't know. Don't have sex with more than one partner. The risk of couples who only have sex with each other getting hepatitis C through sex is low.
Aug. 22, 2025